Worldwide, the incidence and prevalence of irritable bowel syndrome (IBS) are high enough to impact personal lives in various degrees. Whether through psychological effects or social functions, IBS can be troublesome and may occur unexpectedly. For beginners, understanding IBS itself is difficult, as many struggle to grasp how a structurally normal bowel can cause so much pain. This is not surprising, as clinicians and researchers are still trying to fully understand what IBS is and what causes it. As science advances with hopes of understanding IBS completely someday, we are currently left with potential clues about the factors that trigger IBS, namely, a recent history of gastrointestinal infection, certain foods, medications, disruption of the gut microbiota’s ecosystem, psychosocial factors (stresses), and possibly genetics.
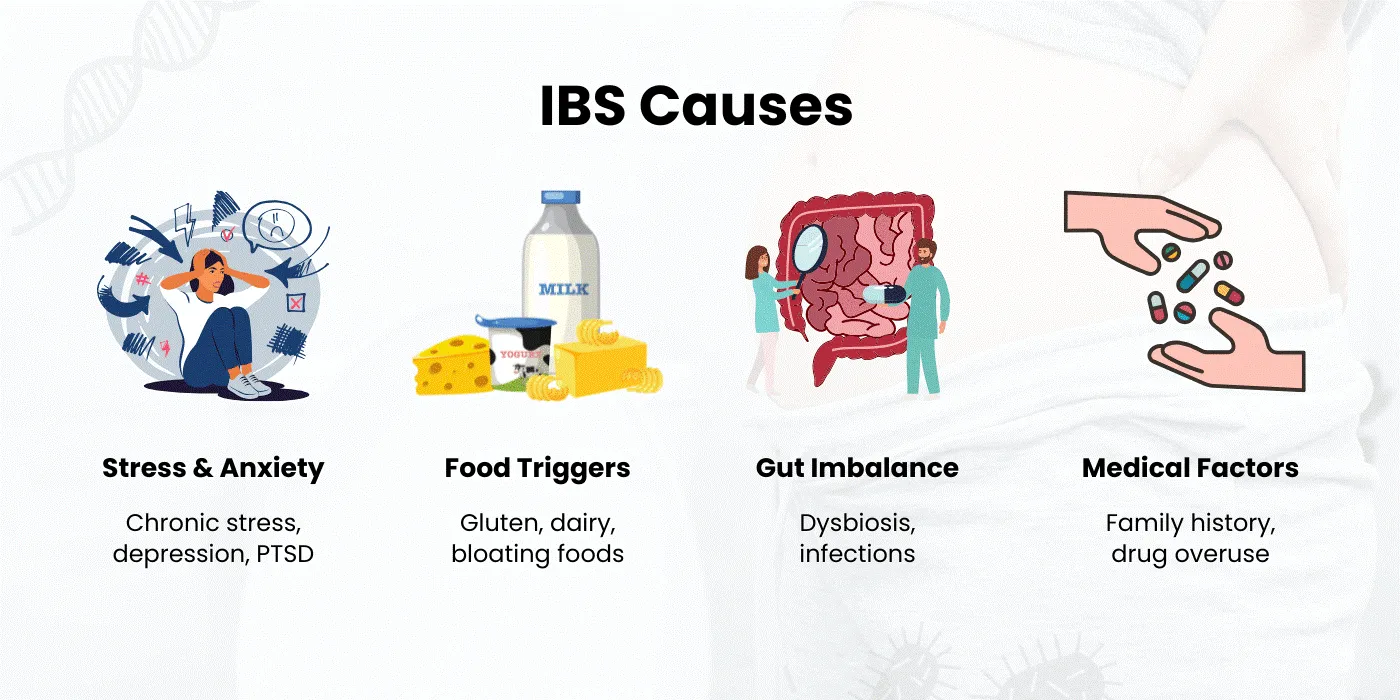
Figure 1: Potential triggers or contributory factors for IBS – current understanding (image courtesy of the PMRI Homeo website).
Among all the possible contributing factors, the psychosocial component is particularly complex. Simply informing the patient that their experience is solely due to stress would not be enough; however, taking a thorough history and establishing a good rapport can help facilitate such a discussion. Following diagnosis, most IBS sufferers require ongoing guidance, patient education, reassurance, and regular follow-up visits whenever symptoms flare up and become difficult to manage.
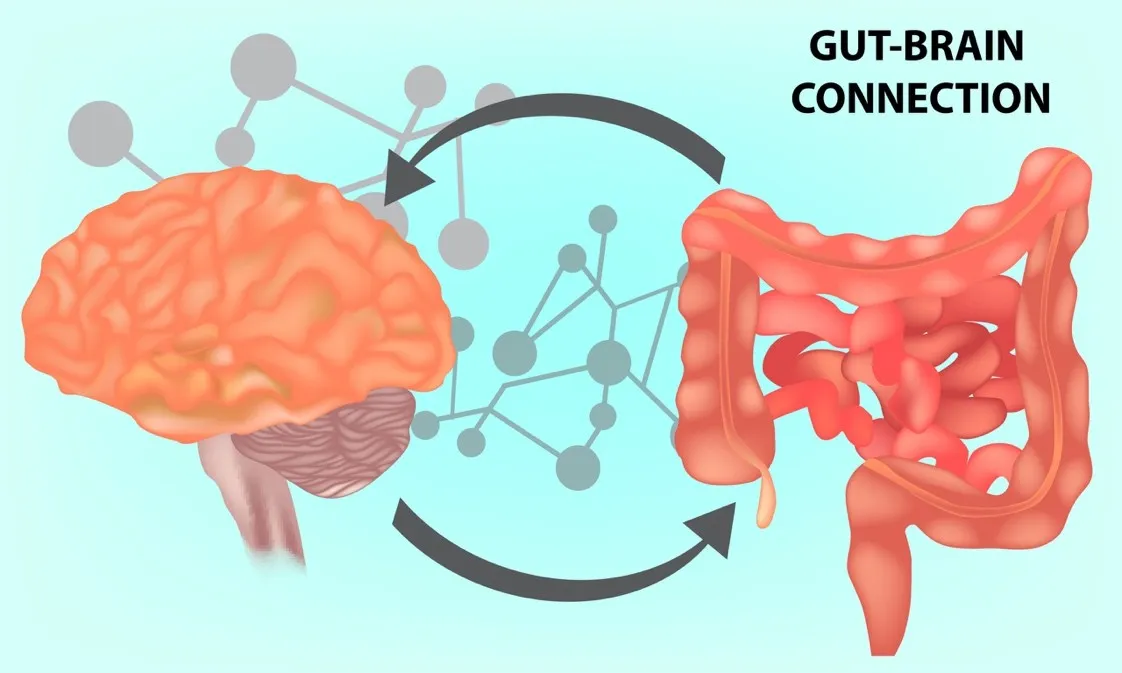
Figure 2: The gut-brain interaction offers a complex interplay of communication that works hand-in-hand to ensure optimal gut function. A problem with the mind will affect the digestive organs, and likewise, a troubled gut will affect the brain (image courtesy of Dr Chiragthakkar’s website).
Madam Tan, a 62-year-old retiree, is one such patient. She has suffered from irritable bowel syndrome for nearly three decades. Her symptoms included abdominal cramps that were colicky, coming in waves, and culminating in a large amount of yellowish watery stools. She was unsure of the cause but observed noticeable relief after defecation. On bad days, these episodes could occur up to six times daily and were unpredictable. The volume of diarrhoea was not always large; sometimes, it was just a few drops of mucus-like stools, but never bloody. Initially, she used over-the-counter medications such as Loperamide and Buscopan. When these proved ineffective, she would visit her GP for intramuscular injections to ease the pain and take Lomotil for several days. Her quality of life deteriorated. She discovered certain foods she could not tolerate, including dairy products, some fruits and vegetables, and mostly beans and nuts. Besides these, many other foods seemed to trigger her symptoms, leading to food avoidance and significant weight loss. Her GP subsequently referred her to a gastroenterologist. She underwent endoscopy and colonoscopy, along with lab tests, ultrasounds, and a CT scan, all of which were unremarkable. Various medications were prescribed, and over the past ten years, she has consulted multiple specialists. Her symptoms tend to improve temporarily but never for long, as they tend to recur weeks after stopping medication. She was told to have IBS and has been prescribed the same medications—antispasmodics (Meteospasmyl or Duspatalin), Loperamide, and recently, multistrain probiotics. Madam Tan now stays mostly indoors, preferring not to attend social functions or go shopping over the weekends, for fear of the unpredictable nature of her IBS episodes.
Clearly, IBS is not just a benign problem; it can escalate to the point of significantly affecting a patient’s quality of life. Although most patients would have some degree of anxiety initially, the troublesome and recurring symptoms they now experience will further intensify their fears. And since IBS is a disorder of the gut-brain interaction, having substantial anxiety benefits no one, perpetuating the vicious cycle of a troubled connection between an already disturbed mind and a confused gut.If it occurs in the elderly, their solitary lives from the empty nest syndrome would only separate them from the community and negatively affect their psyche. If it happens to young individuals who are on the rise in their career ladders, this would be a massive blow to their ability to function at work, missing deadlines, being cut off from potential pay rise and promotion, affecting their self-confidence, and morale.
Miss Ryuku, a 35-year-old financial executive and entrepreneur, is a successful woman. She is a meticulous and systematic planner with a perfectionist mind, an effective worker, and a busy mother of two. Her personal and family life has remained unchanged over the past ten years since she began working and climbing the ranks in her company. However, as she reached a senior managerial level, her job became more demanding. She was frequently required to travel across the state, nationwide, and sometimes internationally, up to twice a week. She tried to keep up with the pace, and although she enjoyed the adrenaline rush initially, she soon burned out. On numerous occasions, she survived on packed meals, instant food, large amounts of cheap coffee, energy drinks, and poor sleep to please her boss and meet her key performance indicators. While this looked good on her CV and her company’s output, she was trading away her peace of mind. A year before she came to my clinic, she began experiencing severe abdominal cramps – first on the right side of her abdomen, then on the left, and occasionally at the bottom. She felt extremely gassy, full despite eating very little, bloated, and sometimes nauseated. These symptoms persisted for weeks, and as she lost her appetite, she started losing weight. A month into her symptoms, she developed, in addition to the initial issues, profuse diarrhoea that, on bad days, could occur 4-6 times a day. The defecation episodes provided relief, allowing her to return to near normal function, but she worries about when the next episode will strike. She was deeply affected and decided to consult a specialist at a separate healthcare centre, where she underwent an endoscopy, colonoscopy, blood tests, and an ultrasound of the abdomen and pelvis; all of which were unremarkable. She wasn't given much information about her condition, but was prescribed Loperamide and Duspatalin for two weeks, which improved her symptoms. However, after stopping the medication, her symptoms returned, initially mild, then with a vengeance. She never maintained her follow-up appointments due to her busy schedule, eventually giving up seeking further treatment, believing this was her new normal, and that she just had to live with it.
Miss Ryuku need not suffer. Modern research leading to a better understanding of IBS has resulted in the development of novel strategies to manage its symptoms—whether through counselling, lifestyle and dietary modifications, probiotic supplementation, medical therapy, or neuromodulators (such as anxiolytics or antidepressants). In Asia, however, the idea of being prescribed neuromodulators is often seen as a stigma, and patients might wonder why the doctor would start them on an antidepressant for a ‘gastric' problem—yet, neuromodulators are among the best drugs to have undergone rigorous trials for various disordered gut-brain interaction illnesses, including IBS. Patients require a detailed, simplified explanation of why these medications become necessary when their IBS symptoms no longer respond to other treatments, how they help in remodelling or repairing nerve sensitivity over time, and, most importantly, that these medications are not necessarily required long-term. While prescribing neuromodulators may seem straightforward, it is equally important to reassure the patient, support them when they develop side effects, provide a clear explanation, and outline an exit strategy. Some patients, however, might require further management through collaboration with GI psychologists, psychiatrists, and dietitians. So, do keep an open mind when your gastroenterologists broach the topic of mental health. We are, after all, living in a fast-paced era where everyone is too busy taking care of everything else, except for themselves.
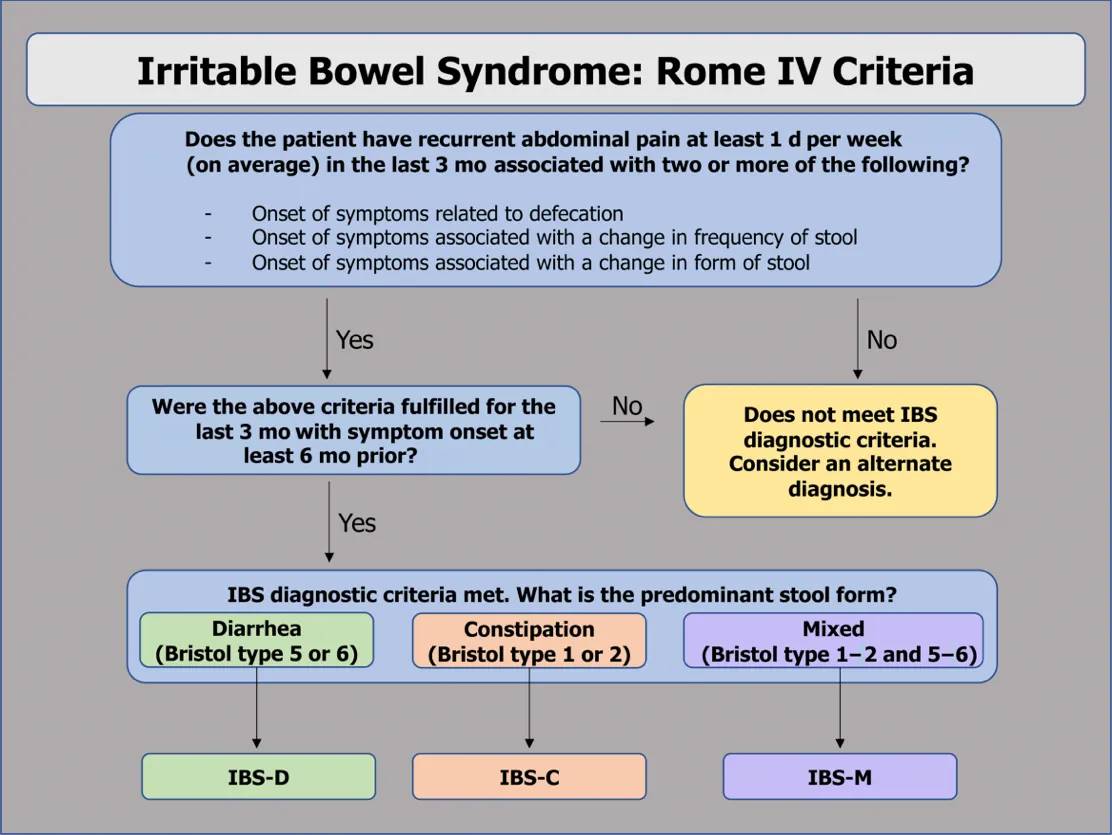
Figure 3: Workflow sheet demonstrating the Rome IV diagnostic criteria for the various subtypes of irritable bowel syndrome (image courtesy of the emorymedicine website).
Not everything is IBS, however. We need to be aware that other conditions can also affect your gut. Some symptoms may not last long enough to raise concern, while others may last longer or be more serious. Physicians use a workflow chart to help determine the diagnosis of IBS (see Figure 3). Of greatest importance are the duration of the symptoms, their frequency and intensity, and the often fluctuating nature of the symptoms with a clear-known trigger.
Your doctor will be able to piece the puzzle together as he guides you through a thorough history-taking. Some of the questions to expect from the doctor that may help you prepare for the consultation include the following:-
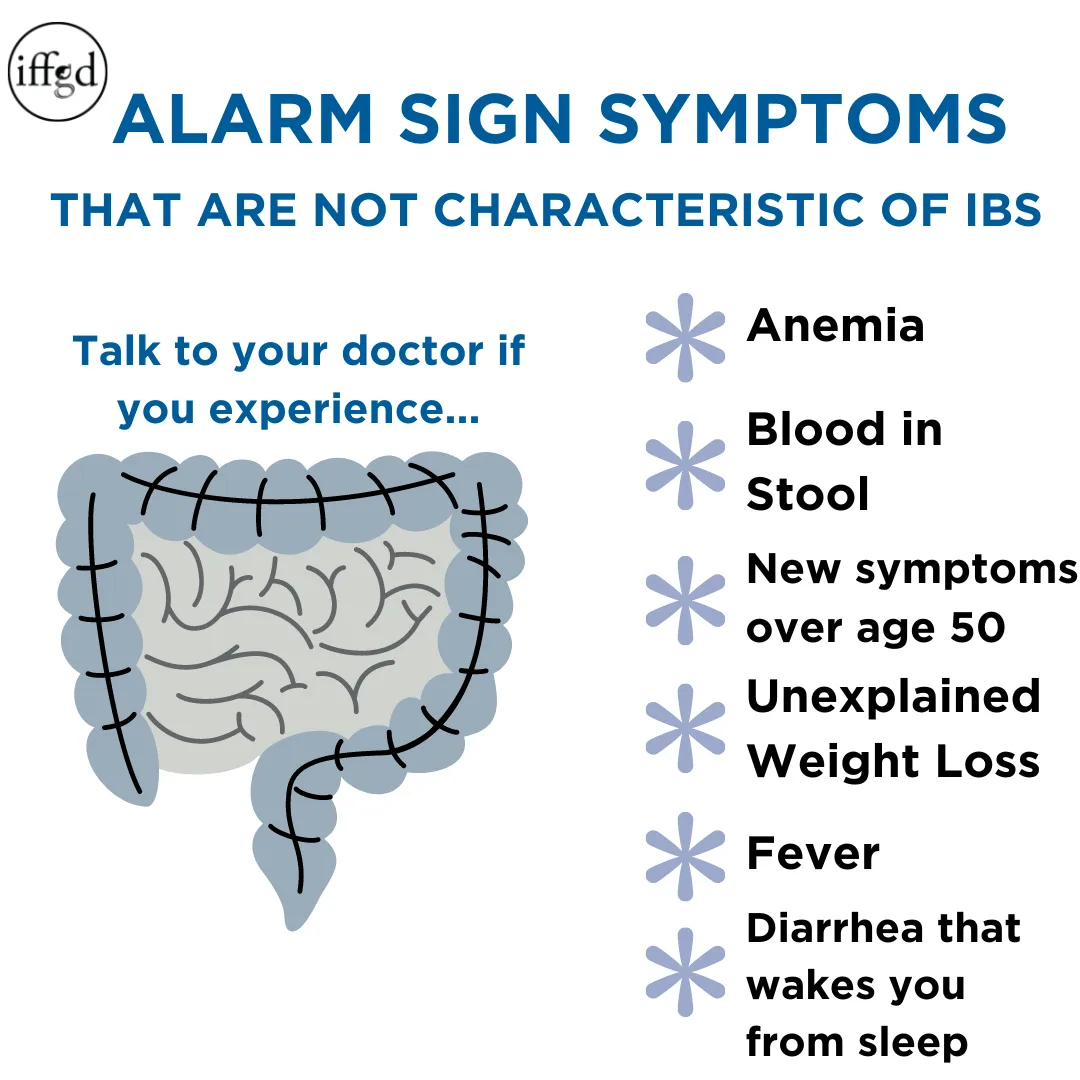
Figure 4: Red flag symptoms that you must not forgo as such symptoms distinguish IBS from other, more sinister pathologies, e.g. inflammatory bowel disease, chronic gastrointestinal infection, and colorectal cancer (image courtesy of the aboutibs.org website).
A patient with undiagnosed IBS would undergo a comprehensive laboratory assessment, including blood and possibly stool analysis. Depending on the patient's age, underlying risk factors, and family history of gastrointestinal malignancies, further evaluation with ultrasound, endoscopy, and colonoscopy may be decided upon on a case-by-case basis.
Strategies for Managing IBS and Improving Quality of Life
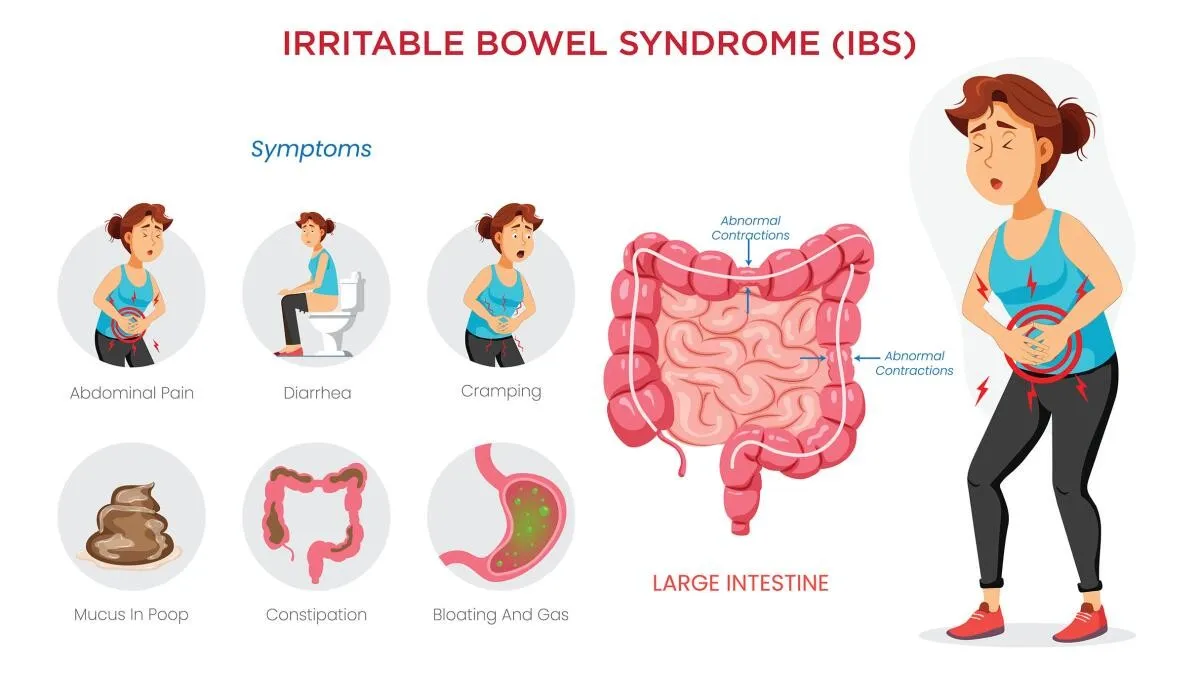
Figure 5: Common symptoms of irritable bowel syndrome – recognising your usual symptoms helps in identifying what triggers them (image courtesy of The Los Angeles Times website).
One of the first steps in managing IBS is to identify personal triggers. Specific foods, stress, or lifestyle habits often provoke IBS symptoms. Keeping a detailed diary of meals, symptoms, and activities can help pinpoint patterns. Once triggers are identified, you can work toward minimising or avoiding them.
With this information, you can work with a healthcare professional to create a personalised plan. We know how difficult this is, especially in Penang, a food paradise, but if you make an effort to be mindful of your diet, positive outcomes are likely to follow.
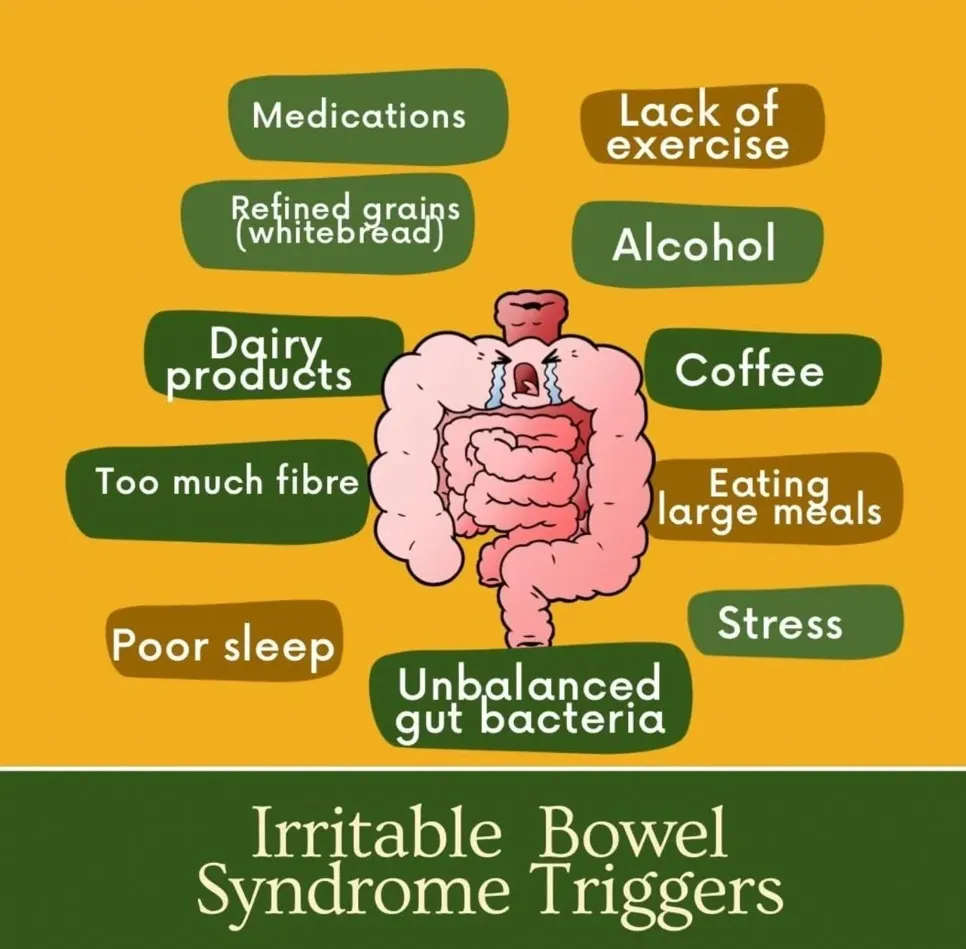
Figure 6: Potential triggers for irritable bowel syndrome, not everyone is the same – familiarise with what your known precipitants are and work towards minimising them to alleviate symptoms.
Diet plays a crucial role in managing IBS symptoms. While triggers can vary, specific dietary adjustments are commonly recommended:
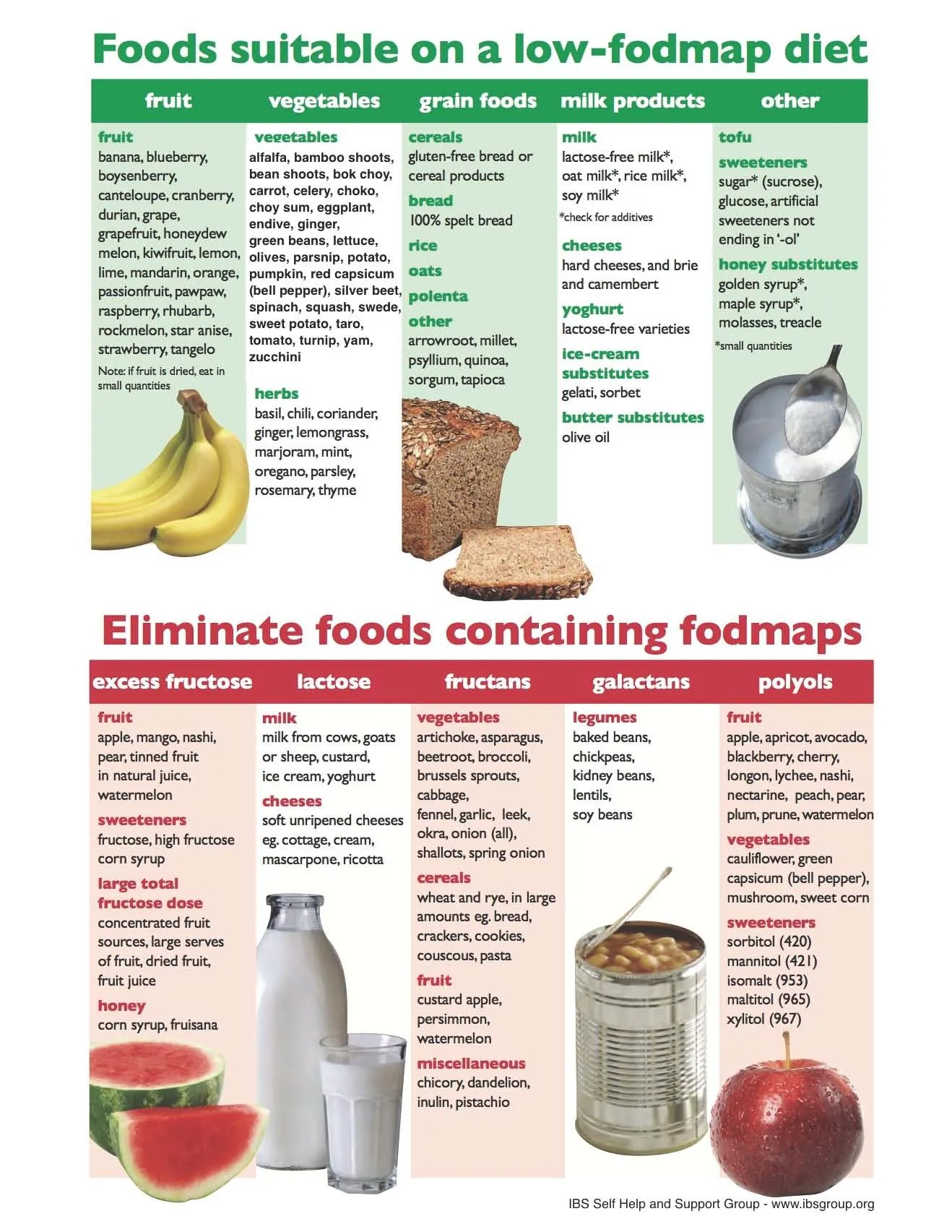
Figure 7: Non-exhaustive list of the FODMAP diet where patients can practice mindful eating and record their daily food consumption alongside symptom development (image courtesy of the IBS group website).
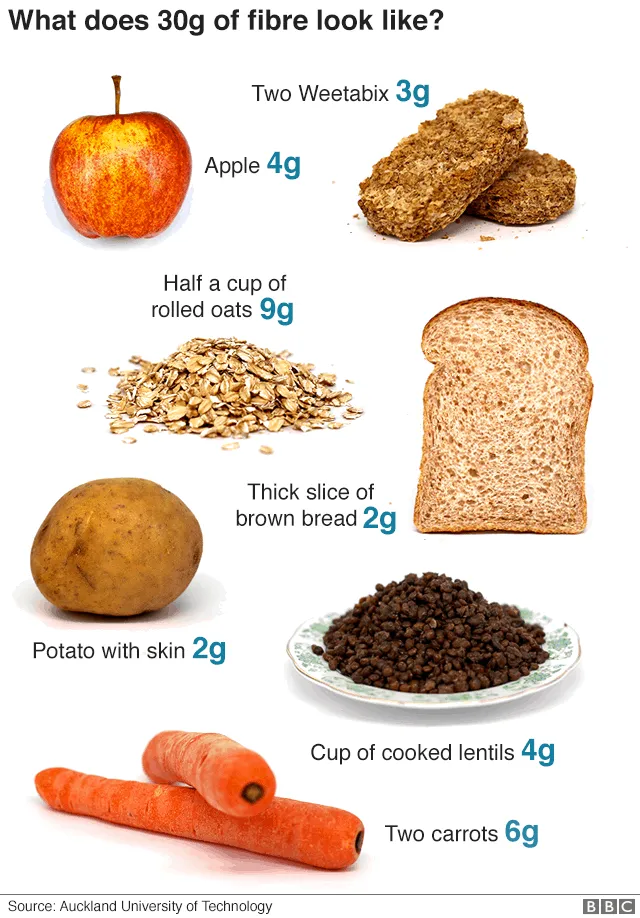
Figure 8: A good illustration of what 25-30 grams of soluble fibre intake per day looks like. With plenty of information available online, creating such meal planners is relatively straightforward (image courtesy of the Auckland University of Technology website).

Figure 9: Processed and ultra-processed foods are known to disrupt the gut microbiome by causing inflammation, and are themselves high in FODMAPs. These foods lack soluble fibre, and in contrast, are rich in emulsifiers (food stabilisers) and sugar that can promote and propagate gut irritation and inflammation.
Stress is a well-known aggravator of IBS. Incorporating stress management techniques can help ease symptoms and improve overall health.
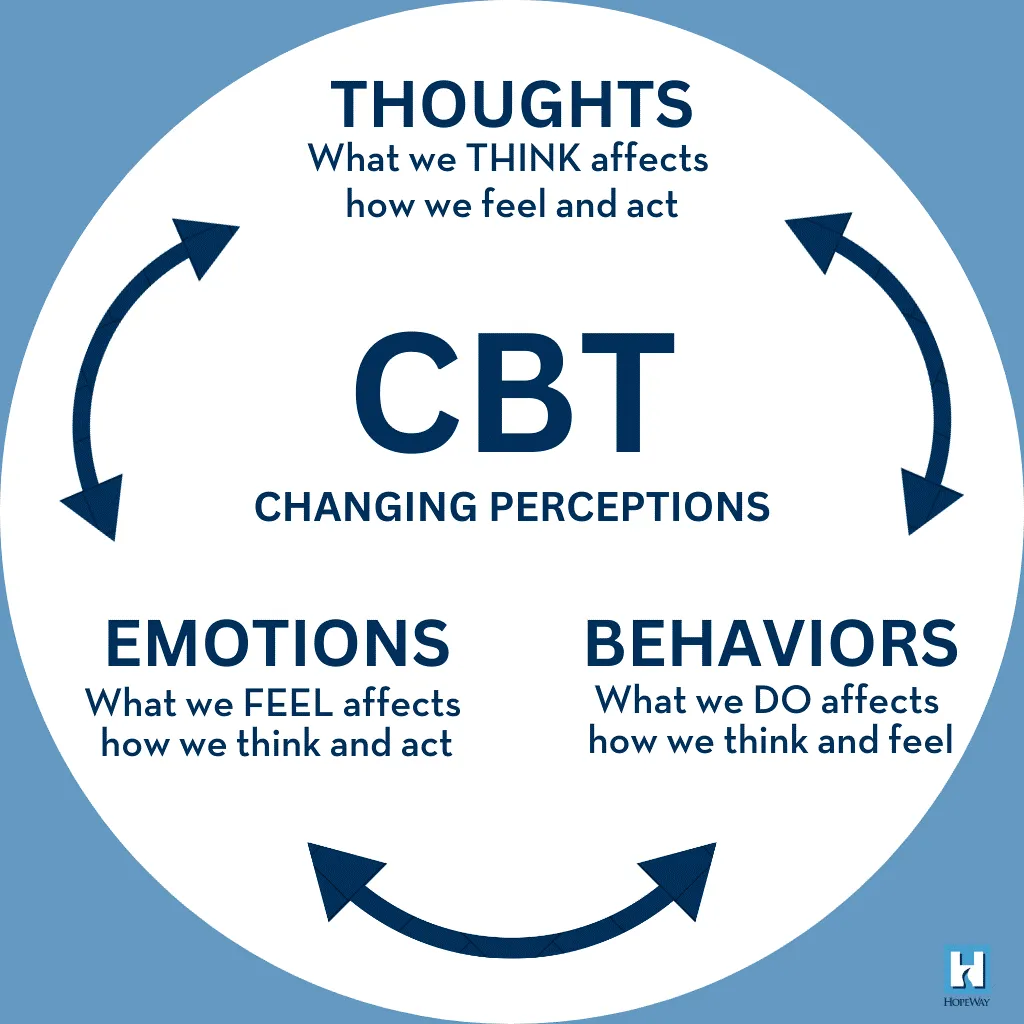
Figure 10: Cognitive behavioural therapy concentrates on the patient’s thoughts, actions, and behaviours. By understanding how a patient responds to situations, the therapist can help them identify and modify their negative thoughts and behaviours to enhance their emotions, mood, and overall functioning (image courtesy of the hopeway.org website).
For some, dietary and lifestyle interventions may not be enough. Several over-the-counter and prescription options are available:
Figure 11: Duspatalin – one of the commonly prescribed antispasmodic agents for IBS in Malaysia (image courtesy of MIMS Malaysia website).

Figure 12: HEXBIO MCP Granule, a locally produced multi-strain probiotic that can be used as an adjunct treatment for IBS of all subtypes (image courtesy of the brcobes.com website).
Despite the various options for pharmacotherapy, it is imperative to consult a healthcare professional about medication choices to ensure safety and effectiveness.
Cultivating daily habits that support your digestive system can lead to sustainable symptom relief:

Figure 13: Set a timer for 15-20 minutes if needed, sit down rather than stand, focus on your food without distractions (no phones, no books, no work, and no TV), eat with friends or family, take sips of liquids between bites, chew thoroughly, and dedicate a specific time for your meals so you do not go hungry or rush through your food quickly.
Successful IBS management often involves teamwork. Stay in regular contact with your healthcare provider, especially when symptoms change or new issues arise.
Complementary approaches may provide additional relief for some people:

Figure 14: Peppermint oil and caraway seed oils are antispasmodic agents that help to reduce symptoms of abdominal pain, cramps, bloating and excessive gas. They are unfortunately not available in Malaysia. They are sold over-the-counter in countries like Australia, the UK, and Canada. Whether these supplements can be purchased through various e-commerce platforms is another matter entirely. Be sure to do your own research before making a purchase online (image courtesy of ca.naturalfactors.com website).
IBS research is ongoing, and new management strategies are continually emerging. Take an active role in your care:

Figure 15: Always remember your red flags and know when it is not IBS (image courtesy of the North Kansas City Hospital’s website).
While IBS can often be managed with lifestyle and dietary changes, specific symptoms require prompt evaluation by a healthcare provider:
These could indicate conditions other than IBS and warrant medical attention.
Living with IBS presents daily challenges, but with the right knowledge and proactive strategies, it is possible to reduce symptoms and enjoy a better quality of life. By recognising your triggers, tailoring your diet, managing stress, and working closely with your healthcare team, you can effectively take control of your IBS. Remember, patience is key—improvement may be slow, but persistence ultimately pays off. Take small, manageable steps and celebrate your progress along the way.