Constipation is a frequent digestive complaint that can affect individuals of all ages. While often seen as a minor issue, persistent constipation can reduce quality of life and may point to more serious health concerns. Patients would try over-the-counter medications first before seeking help from their GPs, while some may even look for help from various social media platforms and make purchases of guaranteed fiber drinks that would help alleviate their constipation. Some may go for more radical approach by undergoing colon cleansing – be it chemically-induced or unproven strategies. As benign as a few laxative tablets may seem, such medications or supplements may turn addictive and serve as a convenient go-to quick aid when help is needed. For most working adults, that is the best approach as long as it still works and gives relief. In the end, when they run out of options, or when their symptoms become prolonged with no solution in sight, some form of irreparable damage might have occurred.
As with my previous articles, allow me to share cases on the various subtypes of functional constipation that we commonly encounter in the gastroenterology clinic. Constipation related to colon cancers have been discussed at length in a separate article and we shall not address them in detail here.
Case Scenario 1
Kumar, a 25-year-old technician, presented with constipation symptoms over eight months. If he were able to recall exactly, it all happened suddenly, with a robust turn of event from normal daily bowel movements, to one that he has to wait for as long as a week before he could get something out from the rectum. During the interval between these pooping episodes, he would complain of slight abdominal discomfort, abdominal fullness, slight distension towards the evening, and tummy cramps following his meals. On those days when he finally goes to the toilet, he would spend up to thirty minutes on the throne and only managed to push out a few hard lumps. There were times when he felt the incomplete sensation following defecation, and that he would insert his fingers to dig or even turn up the water jet to hose his rectum. Neither strategy helps, and the rectum was surprisingly empty. He has resorted to taking various laxatives in syrup and tablet form, tried putting in enemas once to twice a week, and lately, got some traditional herbal drink off an influencer in social media. The latter apparently helps, but over the past 3-4 months, he found himself reliant on it and cannot go without it. His colonoscopy was unremarkable, and he is due for a comprehensive anorectal functional and motility testing.
Case Scenario 2
Uncle Cheng, a 65-year-old retiree, has been living with constipation for over twenty years. During that time, he has had countless doctor consults, four colonoscopies, various laxatives, and consumed many unconventional supplements / herbs, all to no avail. He brought all his results to my clinic and I spent an hour going through all of his symptoms, and found that he would actually try to go to the toilet every day. In fact, he has the urge to pass motion every day, more than what was conventional. During such urges, he would answer the call of nature promptly. He would rush to the toilet, sit down, and start to bear down, only to be disappointed that nothing would appear, but a gush of flatulence. He does not have any tummy discomfort, and he enjoys eating with no recent weight loss, too. He lives a comfortable life and is moderately sedentary. I do notice one thing that he is hiding throughout the interview, and that he was a generally anxious person. I delved deeper into that and found that there were a lot more underlying social issues. I suggested a series of functional studies to investigate the motility, sensation, and strength of the anorectal muscles, to which he was more than happy to participate. Turns out, he has what is called a rectal hypersensitivity issue and dyssynergic defecation. In short, he has a heightened sense of emptying his bowels, and a loss of coordination between the muscles involved in defecation.
Case Scenario 3
Linda, a bright 27-year-old lady, presents with chronic abdominal pain and constipation over three years, which has progressively worsened over three months. She would only go to toilet once a week when she develops intolerable abdominal pain and bloating, and would spend more than half-an-hour straining with some of these occasions complicated with minor rectal bleeding. She has tried various laxatives, and although they do work early on, these medications have been frequently supplanted by newer agents. A recent colonoscopy along with blood tests were unremarkable, and she objected to further functional studies. Nevertheless, her symptoms were in keeping with irritable bowel syndrome of the constipation subtype, given the duration of illness and the frequency of symptoms recently. She was counselled on her issues, and started on appropriate medications for irritable bowel syndrome, gut-selective antibiotics, and probiotics. And although her symptoms have begun to improve, she would still require follow-ups to ensure that she do not regress, in which case, neuromodulators would be the next best option.
Case Scenario 4
Pamela, a 30-year-old foreigner, was in Malaysia for studies. She has been suffering from chronic constipation for over 15 years and has tried various lifestyle modifications, increased consumption of fiber, taking laxatives, prokinetics, secretagogues, enemas, and undergoing biofeedback therapy, none of which work for long. In the matter of that duration, she has done way more tests than Uncle Cheng (Case 2), and found that she has slow-transit constipation with a minor component of irritable bowel syndrome. In slow-transit constipation (also termed as lazy bowel syndrome), Pamela’s large bowels move extremely slow and she would only develop the urge to answer nature’s call once a month. Radical options were discussed from her home country, and this involved the total removal of her large bowel, and reinstituting bowel continuity by connecting the small bowel to the rectum. Having considered her options, she has decided to continue with what she is presently doing, and reserve such aggressive intervention to a later stage. An option of fecal microbiota transplantation was discussed with her where healthy donor stools are transferred into the patient’s gut with hopes in restoring a healthy balance of gut microbiome (probiotics) and thus palliate her symptoms.

Figure 1: Fecal microbiota transplant in progress in a patient of mine – a routine colonoscopy is first performed followed by spraying of the fecal content into the patient’s small and large bowel.
Fecal microbiota transplant is an expensive procedure and is not covered by medical benefits or insurance, and our patient is not keen to undergo such tests where there is no full guarantee on a positive outcome. We do however have other patients who experienced favourable prognosis and have been doing well without laxatives.
Having shared the common clinical scenarios above, let us now delve into exploring further on the formal aspects of constipation; its’ causes and symptoms, recommended investigations, effective prevention and management strategies, and when to seek professional help.
Constipation refers to infrequent, hard, or painful bowel movements, typically defined as having fewer than three stools per week. However, “normal” can vary greatly between individuals. People with constipation may describe hard or lumpy stools, straining, bloating, or a feeling of incomplete evacuation (tenesmus). The Bristol stool chart is an excellent reference chart to guide your doctor in understanding your condition. Be sure to highlight your baseline and current stool form and shape. Such abrupt or gradual change helps point to certain conditions.
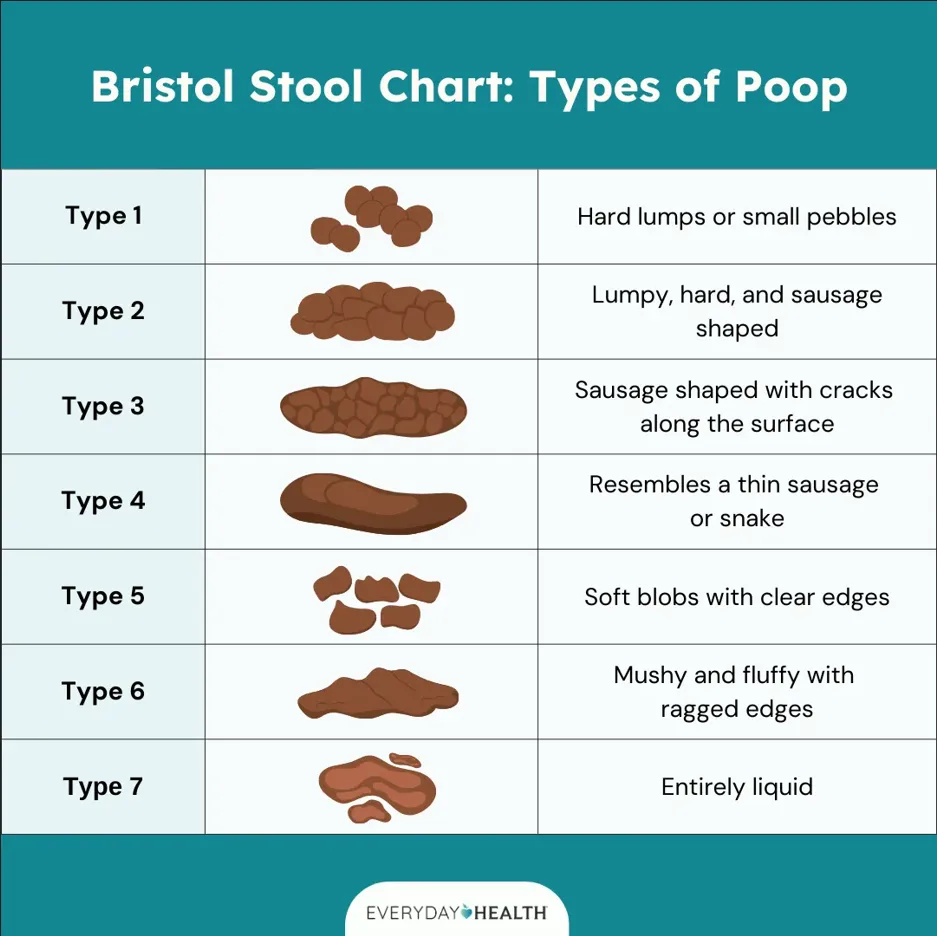
Figure 2: A formal illustration of the Bristol stool chart which clinicians and nurses use to classify the various type of stool shape and form. Patients find this graphic imagery useful than just wordy description. Communication between doctors is also eased through this formalized stool chart (image courtesy of the Everyday Health website).
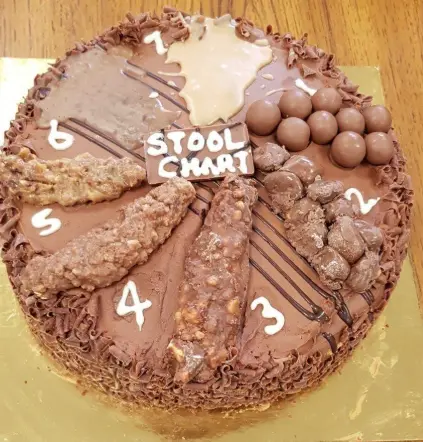
Figure 3: A more informal and hilarious stool chart aimed at younger patients to ease discomfort and anxiety in the clinic (image courtesy of the Institute of Biomedical Science, UK).
Constipation may be caused by:

Figure 4: An illustration depicting a list of top ten causes for constipation – most opinions bank on the lack of fluid intake, poor dietary fiber consumption, living a sedentary lifestyle, concomitant medical conditions and medications that affect the gut motility, and as well as gut dysbiosis (image courtesy of gidoc.co.za website).
Common symptoms include:
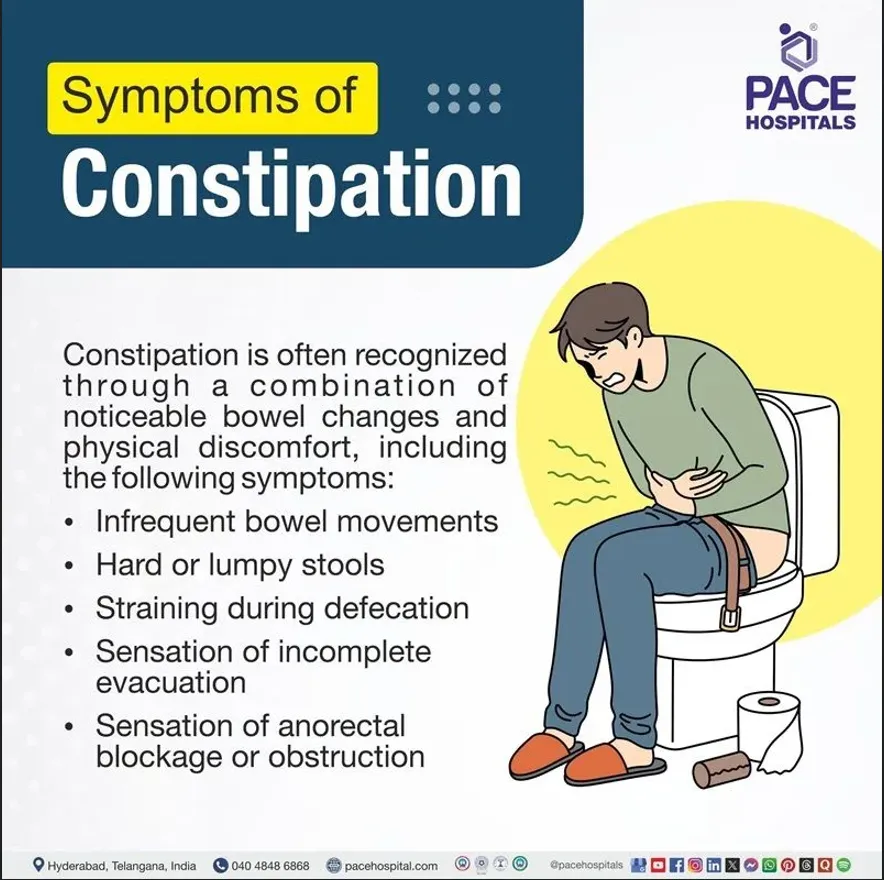
Figure 5: An illustration on the common symptoms encountered in constipation (image courtesy of the PACE Hospitals website).
While many cases of constipation can be managed with lifestyle modifications and do not require extensive testing, certain situations—such as severe, persistent, or unexplained constipation—warrant further investigation. The following diagnostic approaches may be used:
In general, a doctor will start the consultation by asking you to describe your symptoms. Certain tips to prepare yourself ahead so that the consultation will be fruitful include:
The duration of your symptoms – when it first started, how frequent do you go to the toilet to defecate in a week, and how much has this frequency changed compared to before the onset of constipation.
The progression – since constipation developed, have you notice a worsening in terms of the reduction in frequency of your bowel movements, and the need to adopt extra measures to encourage defecation.
The intensity – describe how long you need to be in the toilet, efforts required to strain, manual digitation through putting fingers into the rectum to dig out fecal matter, or using of a water hose to try to empty the rectum.
Other related symptoms – any bleeding, sensation of incomplete evacuation, a sensation of a mass coming out during passing motion, or mucus discharge. It would also help to describe whether there is any associated abdominal pain, discomfort, and bloating, or a sensation of a mass on your tummy. Whatever you feel abnormal and that comes with each episode of constipation bout, please highlight this in your notepad and discuss it with your doctors. Irritable bowel syndrome for example can coexist with other functional gastrointestinal disorders.
Lifestyle alteration – it helps the clinicians if you could also include in your description that you have tried changing your lifestyle, that you have increased your physical activities through exercises, drunk more than 2 to 2.5 liters of water a day, take loads of fruits, fibers and vegetables, and cutting down red meat and processed foods. If you have previously taken medications for coexisting medical conditions, please bring them. If there are any recent short term medications that you have taken such as antibiotics, pain killers, or opioid-related drugs, please disclose them, as it helps us to understand the reason behind certain causes of constipation that may be short-lived.
Measures taken – whether you have taken laxatives, syrup or tablets, enemas or suppositories, herbal or traditional, special juices or unlicensed supplements. Bring labels or boxes if you cannot pronounce the names. Recall the duration that you take these medications, how did you come about it, why did you stop it, and if there is a switch to another class or group, knowing the reason behind this helps in formulating a strategic plan later on.
Family history – constipation runs in the family, if you have multiple family members who experienced the same issue and that you have tried everything, perhaps we are dealing with gut dysbiosis. Your doctor may delve deeper into the psychosocial aspects of your life, too, if a functional cause is likely. Remember, anxiety and depression may also lead to altered gut motility and contribute to constipation. Do maintain an open mind when the topic eventually veers this way. After all, we are living in a stressful, fast-paced, and ever-changing era.
Following detailed history taking, doctors would perform a thorough clinical assessment by examining the relevant areas of your body. In certain cases, a digital rectal examination is mandatory especially when you describe symptoms of rectal bleeding, mucus discharge, feeling of incomplete evacuation, or a mass sliding out and then going back in during defecation. In such instances, the doctors will be gentle, and apply a generous amount of lubrication before inserting his fingers. A general inspection of the anus and perianal region will be conducted first before the digital assessment. You will be given tissue papers or wet wipes to clean yourself. A chaperon/assistant of the same gender with the patient will be available at all times during the examination.
Your doctor may proceed to ask you for further tests to assess for associated conditions and these may include
In certain cases, especially when warning signs or red flags appear (see my previous article on Colorectal Cancer), an imaging and endoscopy may be conducted.

Figure 6: Case of acute constipation with severe abdominal pain in a young lady – CT scan of the abdomen and pelvis revealed impacted stools with gas shadowing (yellow arrow), classical for fecal matter. Patients often present in the emergency department out of severe pain and has often tried numerous remedies be it, over-the-counter painkillers or laxatives, and visited her GP several times for analgesic injections.
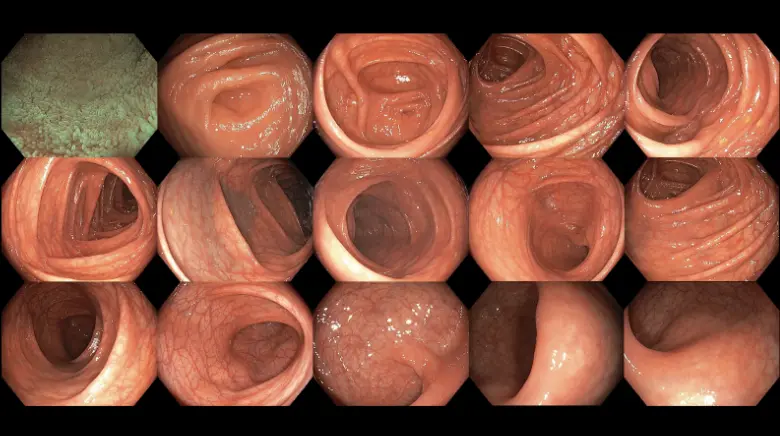
Figure 7: Colonoscopy is useful in detecting colon cancers, one of the causes for chronic constipation.
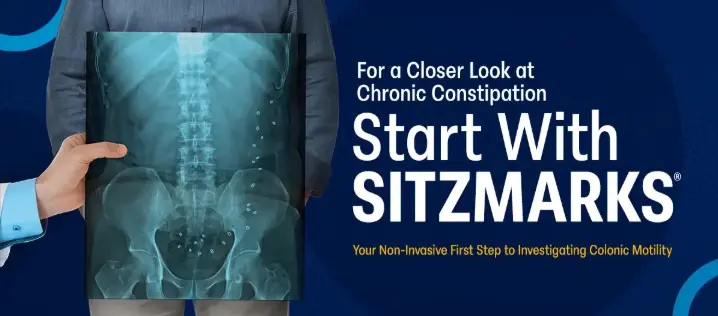
Figure 8: The Sitzmarks capsule study is a practical, safe, and cost-effective tool to assess constipation subtypes – colonic motility issues (slow-transit constipation) or anorectal muscular dysfunction (dyssynergic defecation). After swallowing the capsule, an abdominal X-ray is taken after five days to examine the number of rings remaining and their distribution (image courtesy of the Sitzmarks.com website).

Figure 9: An abdominal X-ray taken at day 5 following Sitzmarks capsule ingestion in a patient of mine diagnosed with dyssynergic defecation. Notice how all the radio-opaque rings are scattered towards the left-sided large bowels, with a few more in the pelvic cavity. Some rings are seen in the right-sided colon as well, denoting that our patient might also has concomitant slow-transit constipation.
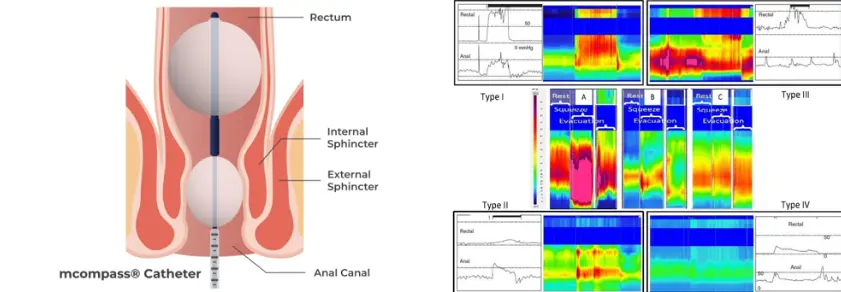
Figure 10: Image illustrating how anorectal manometry is performed (left) and the data analysis afterwards (right). Such assessments enable the clinician to identify the subtype of constipation caused by discoordination between the rectum and anal muscles, thereby guiding the most appropriate treatment options (image courtesy of the Medspira website and Lee et al. Journal of Neurogastroenterology and Motility 2018).
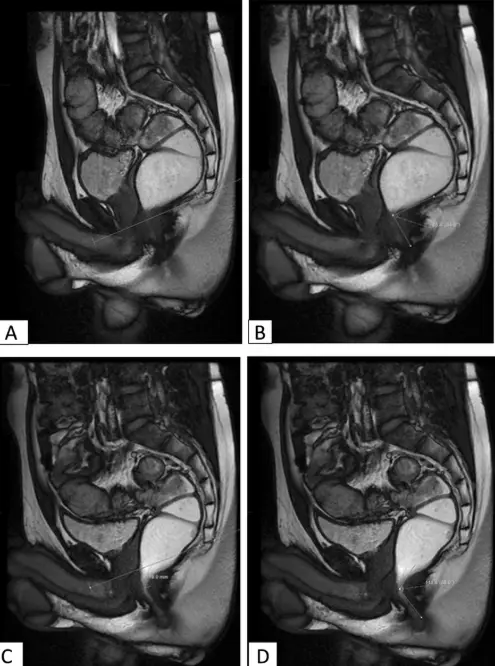
Figure 11: An illustration of how MR defecography is performed to evaluate pelvic floor function, and to identify any structural or anatomical abnormalities contributing to defecation disorders (image courtesy of Saraya et al. Egyptian Journal of Radiology and Nuclear Medicine 2020).
Investigations should be considered when:
Untreated constipation can lead to:
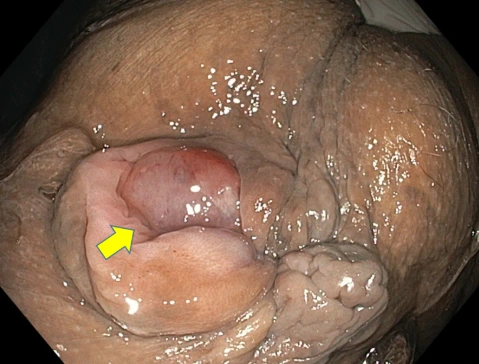
Figure 12: Prolapsed internal haemorrhoids (yellow arrow) in a patient with chronic constipation.
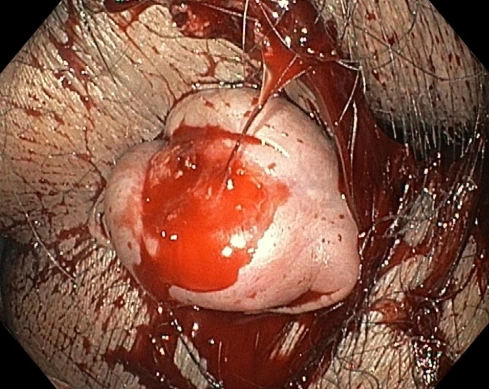
Figure 13: Bleeding internal haemorrhoids resulting from excessive straining and severe constipation.
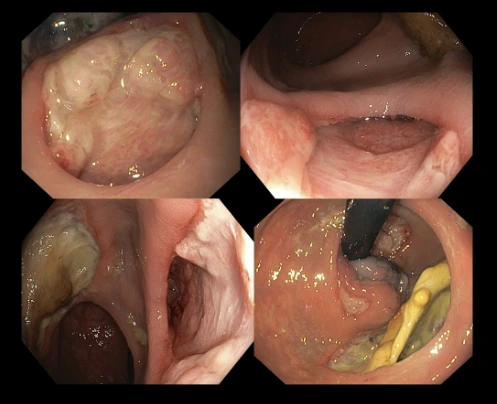
Figure 14: Botched hemorrhoidal surgery in an unlicensed outlet offering guaranteed outcome through non-operative means. The patient presented with chronic rectal discharge, bleeding, and severe pain a week following the outpatient treatment received from the clinic. A colonoscopy revealed large ulceration denoting recent procedures performed, the location of these ulcers were far away from the area where the haemorrhoids were supposed to be. Further to this, a fistula – an abnormal connection between the rectal walls and the perianal region (where fats are located) has formed leading to pus collection and infection. An MRI confirmed all these findings and the fistulous connection resulting from a through-and-through tear (perforation) from the lining of the rectum to the peri-rectal fat.
Key strategies include:
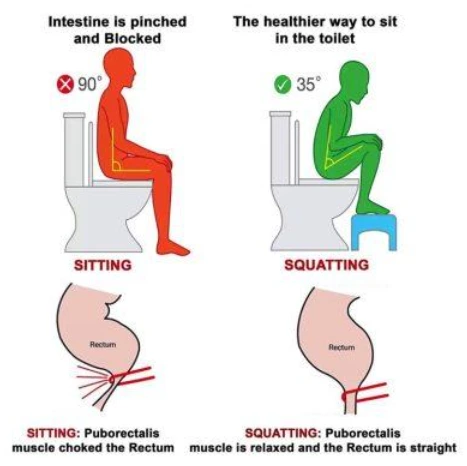
Figure 15: Perhaps an understatement or a frequently overlooked home remedy for proper defecation posture is to place a stool at the bottom of your seated toilet and place both your feet on it to straighten the anorectal path. Such measures ease the passage of stool movement by relaxing the puborectalis muscles (see diagram) (image courtesy of the MOTI physiotherapy website).
Seek prompt care if you experience:
Your physician may suggest investigations as outlined above to better understand and address your symptoms.
Older adults are at increased risk due to reduced gut motility, multiple medications, and reduced activity. Diet, hydration, movement, and medication review are essential.
Hormonal shifts and a growing uterus can slow digestion. Pregnant individuals should prioritize fiber, fluids, and gentle activity with healthcare guidance.
Figure 16: Everyone is entitled to their own opinions, but not every opinion is factual. Fact check with proper sources before adopting it as a lifestyle measure. What works for one individual, may not work for another.
Constipation is a common but manageable digestive concern. Recognizing symptoms, understanding causes, and knowing when and how to investigate are key to effective management. If you experience persistent or severe symptoms, seek advice for appropriate evaluation and treatment. Adopting healthy habits supports lifelong digestive health.