What is Anterior Cruciate Ligament Reconstruction (ACLR)?
Anterior Cruciate Ligament Reconstruction (ACLR) is a surgical procedure that replaces a damaged ACL with a strong, healthy graft taken from a nearby area of the knee. This surgery is commonly performed using arthroscopy, a minimally invasive technique where a small camera is inserted through tiny incisions to diagnose and repair the knee.
ACLR is the gold standard treatment for active individuals, helping to:
- Restore knee stability
- Improve functional movement
- Support a safe return to sports and daily activities
Why Apply VDO Framework to ACLR?
At Pantai Hospital Kuala Lumpur (PHKL), we implement the Value-Driven Outcomes (VDO)
framework to enhance ACLR procedures by focusing on:
✔Better patient
recovery and functional outcomes
✔Cost efficiency by reducing
unnecessary expenses
✔Consistent, high-quality care aligned with international
standards
By tracking key outcomes such as knee stability, pain reduction, and return to activity, VDO helps optimize resources, refine surgical techniques, and improve rehabilitation protocols. It also promotes transparency and trust by demonstrating measurable improvements in patient care, making ACLR safer, more effective, and cost-efficient at PHKL.
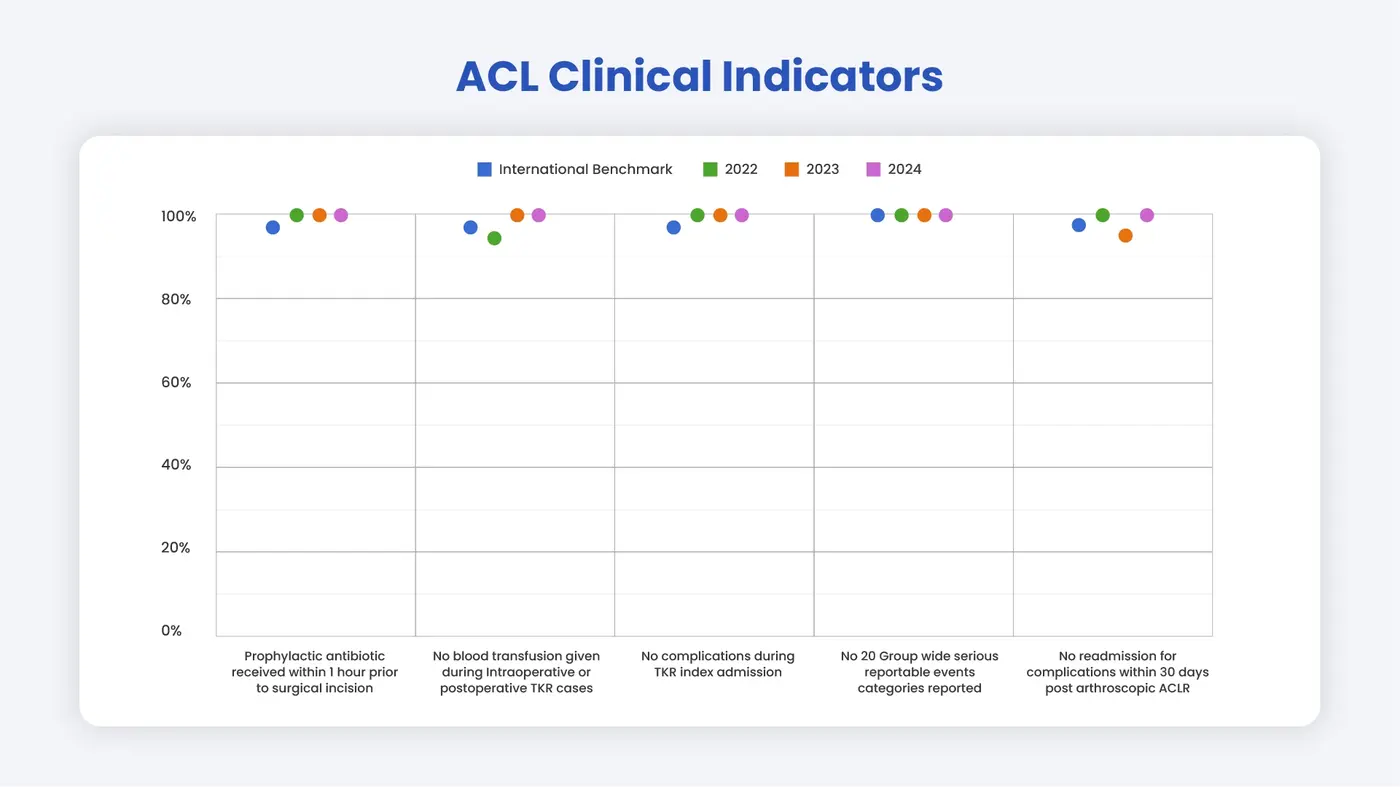
Key Quality Indicators for ACLR Success
At Pantai Hospital Kuala Lumpur (PHKL), we prioritize safety, quality, and optimal patient outcomes in ACL reconstruction. To achieve this, we monitor the following key quality indicators:
- Timely Prophylactic Antibiotics
✔ Patients receive antibiotics within 1 hour before surgery to reduce the risk of infection.
✔ Combined with strict sterile techniques, this significantly lowers the chances of post-surgical infections such as septic arthritis, which can delay recovery and limit mobility. - No Blood Transfusion During or After Surgery
✔ ACLR is a minimally invasive procedure, but managing blood loss is essential.
✔ Avoiding unnecessary blood transfusions reduces risks and promotes a smoother recovery - No Surgical Complications During Hospital Stay
✔ Understanding and tracking ACLR complication rates helps improve surgical techniques.
✔ Identifying modifiable risk factors ensures safer procedures and better patient outcomes. - No Unplanned Readmissions Within 30 Days
✔ This key indicator reflects post-surgical care quality and hospital performance.
✔ While ACLR is generally safe, monitoring readmissions helps identify and prevent potential complications. - Zero Serious Reportable Events (SREs)
✔ PHKL actively reviews and addresses any serious events to enhance patient safety.
✔ By preventing recurrences, we ensure continuous quality improvement and patient confidence.
How does Pantai Hospital Kuala Lumpur compare to international benchmarks?





.webp?sfvrsn=20763f7d_21)


.webp?sfvrsn=f2a2c343_12)


