Colonoscopy Procedure
What is a Colonoscopy?
A colonoscopy is a procedure to examine the inside of the colon (large intestine) and rectum using a thin, flexible tube with a camera. It helps find and remove colon polyps, detect colon cancer early, and diagnose digestive issues. Doctors recommend it for colorectal cancer screening, diagnosing and monitoring gut health, especially for those with risk factors like a family history, inflammatory bowel disease, or previous polyps.
What age should you get a colonoscopy?
Colonoscopy is recommended from age 40 to detect and prevent colorectal cancer early, especially for those at higher risk or with certain digestive and kidney diseases. Cancer rates are rising in younger adults, making early screening tests important. It helps find and remove precancerous polyps before they turn cancerous, lowering colorectal cancer incidence. People with a family history or certain health conditions may need screening even earlier for better outcomes.
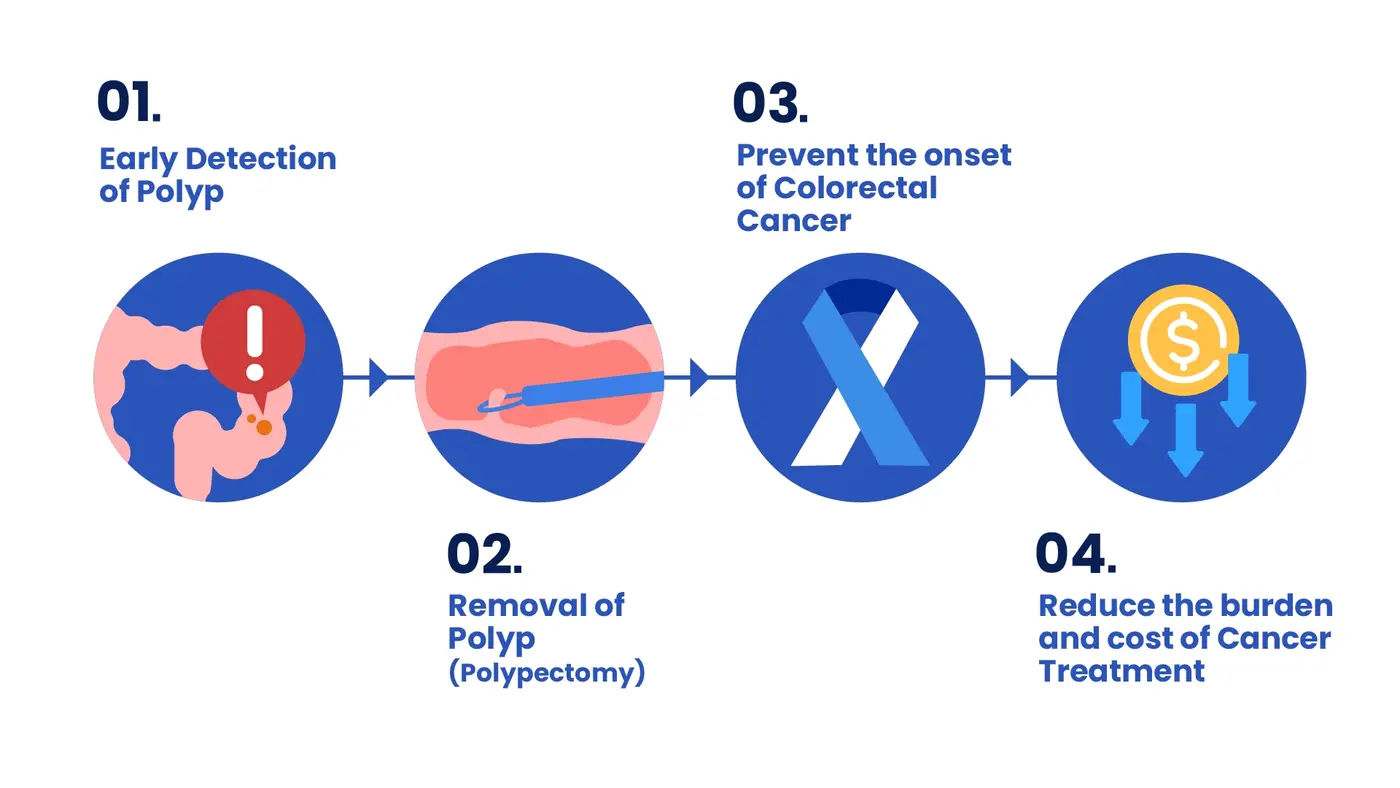
Why Apply VDO Framework to Colonoscopy?
In PHKL, we apply the Value-Driven Outcomes (VDO) framework in colonoscopy to:
- enhance patient outcome
- optimise resource use
- improve overall care efficiency
By analysing data on quality indicators such as detection rates, complication rates, and patient experience, we can identify best practices that lead to safer, more effective procedures. This ensures that patients receive evidence-based care while reducing unnecessary costs.
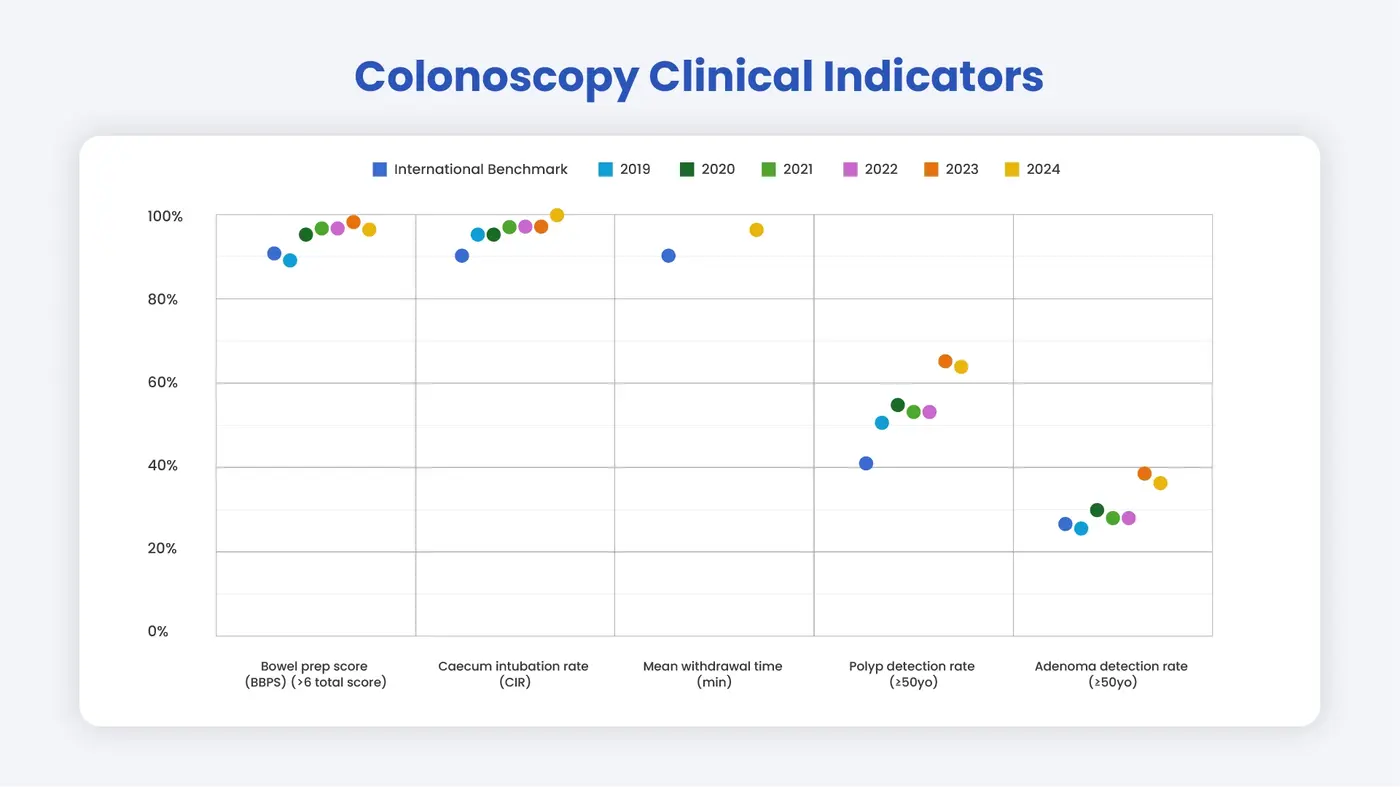
Colonoscopy Clinical Indicators
- Adequate bowel preparation (Boston Bowel Prep Score > score 6 = Good Bowel Prep)
- A poor bowel prep cleanliness caused limited visibility of colon during examination which correlates to the Polyp & Adenoma Detection Rate.
- Caecal intubation rate = ≥ 90%
- The rate of doctor fully inserted the colonoscope into colon to detect any precancerous polyps or lesions.
- Withdrawal Time = ≥ 6 min
- The total amount of time spent during a colonoscopy. A 6-minute withdrawal time is currently the standard of care.
- Polyp Detection Rate (PDR)
- The rate of detecting any precancerous polyp in colon.
- Adenoma Detection Rate (ADR)
- The rate of detecting Adenomas which are generally benign or noncancerous tumour but carry the potential to become adenocarcinomas which are malignant or cancerous.
How does Pantai Hospital Kuala Lumpur compare to international benchmarks?
Additional screening options such as virtual colonoscopy and fecal occult blood tests can be considered for some patients, but a traditional colonoscopy procedure remains the gold standard for examining the entire colon, taking tissue samples, and thoroughly inspecting every segment, from the rectum to the sigmoid colon and beyond. During the procedure, the doctor closely examines the colon wall to look for signs of developing colorectal cancer or other abnormalities.
At Pantai Hospital Kuala Lumpur, we are committed to providing world-class healthcare with a personal touch. Our state-of-the-art facilities and highly skilled gastroenterologists in Kuala Lumpur ensure that you receive the most advanced medical care available. Whether it’s routine preventative screenings like colonoscopies or more complex treatments, we prioritise your health and comfort at every stage.





.webp?sfvrsn=20763f7d_21)


.webp?sfvrsn=f2a2c343_12)


