Laparoscopic Cholecystectomy (Lap Chole)
What is Laparoscopic Cholecystectomy?
Laparoscopic cholecystectomy, commonly known as lap chole, is a minimally invasive surgical procedure to remove the gallbladder—a small, pear-shaped organ located beneath the liver that stores bile, a digestive fluid.
Why is Lap Chole Performed?
Doctors recommend gallbladder removal
for conditions such as:
- Cholelithiasis – Gallstones in the gallbladder causing pain or discomfort.
- Choledocholithiasis – Gallstones in the bile duct, blocking bile flow.
- Cholecystitis – Inflammation of the gallbladder.
- Pancreatitis – Inflammation of the pancreas due to gallstones.
Why Apply VDO Framework to Lap Chole?
Using the Value-Driven Outcome (VDO) framework for laparoscopic cholecystectomy ensures better patient care, improved efficiency, and enhanced quality standards. By tracking complication rates, recovery time, pain levels, and hospital stay duration, we can:
✔Optimize surgical techniques and post-operative care
✔Enhance patient
safety and experience
✔Reduce unnecessary healthcare
costs
✔Ensure transparency and measurable quality improvements
At Pantai Hospital Kuala Lumpur (PHKL), applying the VDO framework makes laparoscopic cholecystectomy safer, more effective, and cost-efficient, ensuring better patient outcomes and international benchmark alignment.
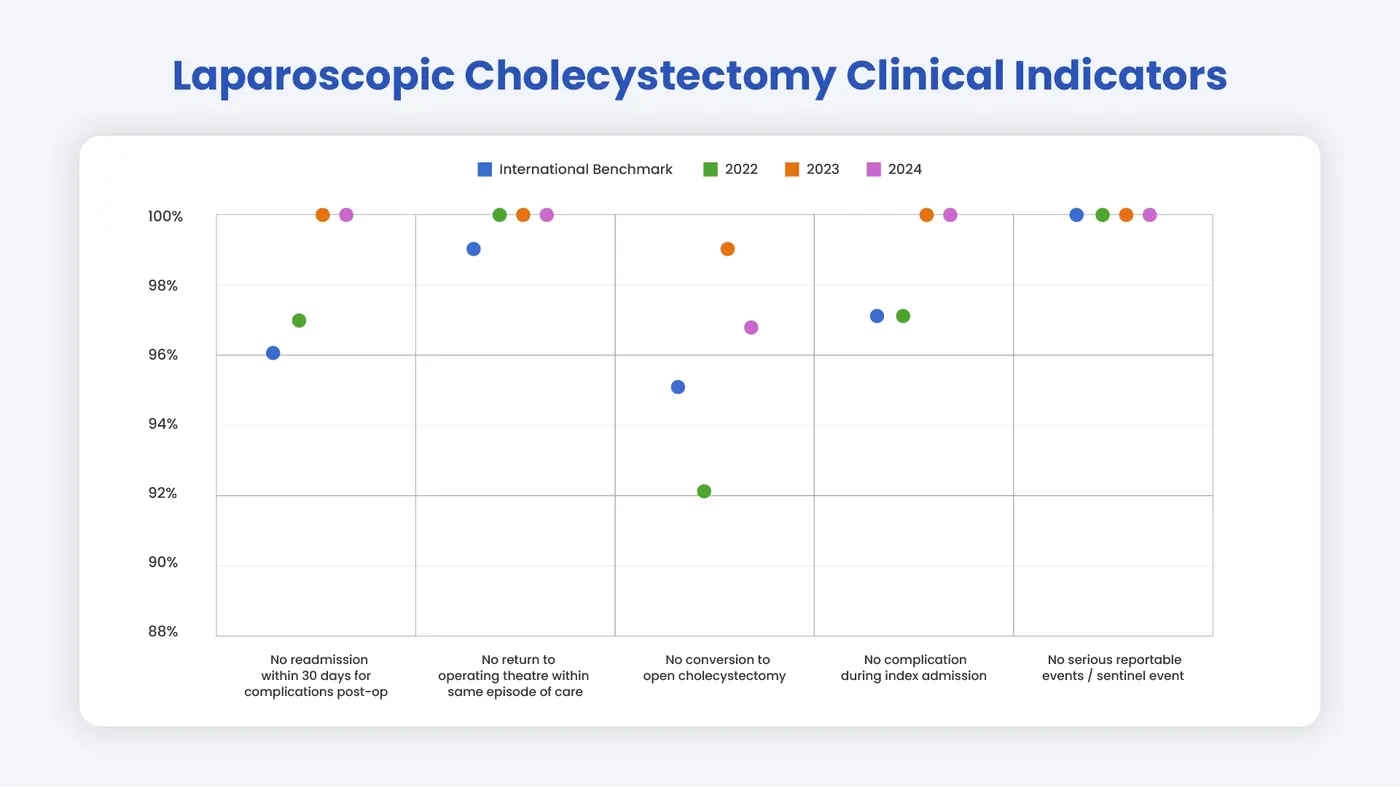
Laparoscopic Cholecystectomy Quality Indicators (benchmarks)
- No Conversion to Open Cholecystectomy
✔ A low conversion rate indicates a successful minimally invasive procedure without the need for an open surgery, reducing recovery time and complications. - No Bile Duct Injuries
✔ Avoiding bile duct injuries prevents serious complications like infection and long-term digestive issues.
✔ This benchmark reflects surgical precision and adherence to best practices. - No Unplanned Return to Operating Theatre
✔ Lap chole is designed to be a safe and definitive procedure.
✔ A low rate of reoperation indicates successful initial surgery and fewer complications. - No Complications During Index Admission
✔ Tracking complication rates helps identify risk factors and improve surgical techniques.
✔ This ensures higher success rates and faster patient recovery. - No Readmission Within 30 Days
✔ A key measure of post-operative success and hospital performance.
✔ Readmissions signal potential complications, so tracking them helps improve post-discharge care. - No Serious Reportable Events (SREs)
✔ PHKL ensures continuous monitoring, evaluation, and corrective actions to prevent serious reportable events.
✔ This fosters cross-learning and ongoing improvements in patient safety.
How does Pantai Hospital Kuala Lumpur compare to international benchmarks?





.webp?sfvrsn=20763f7d_21)


.webp?sfvrsn=f2a2c343_12)


