Figure 1: An illustration depicting the hidden dangers of contaminated food (image courtesy of the emedicinehealth.com website).
Food is an essential part of our lives, nourishing our bodies and delighting our senses. Yet, food can also harbour invisible dangers. Food poisoning, a common yet sometimes serious health issue, can affect anyone at any time. This article delves deep into what food poisoning is, its causes, symptoms, treatment, and, most importantly, how to prevent it.
Allow me to present four distinct case scenarios that seem to recur throughout the years I have been practising as a gastroenterologist. This notion brings me to ponder the statement that the players (the victims/patients) may change, but the game (the pathogens) remains the same.
Sylvester, a 38-year-old man, was enjoying a night out with friends at a local restaurant. He ordered a large serving of delicious Pork Pan Mee with Wan Tan Soup and washed it down with an equally tasty Iced Longan. On his way home, about thirty minutes after dinner, he began experiencing abdominal cramps and bloating. He didn’t think much of it, dismissing it as just some gas he sometimes gets. Besides, it had been a long day, and he hadn’t eaten much, with his Pan Mee being his first meal of the day aside from an iced coffee for breakfast. As he reached home, his stomach started to rebel, and he began feeling nauseous. He barely made it to the bathroom before vomiting multiple times, with all the undigested noodles and longans ending up in the toilet bowl. However, that was not all. He continued vomiting several more times during that hour, and just when he thought it was over, his lower abdomen started growling incessantly. He had to go back to the toilet and began passing large amounts of mushy, foul-smelling stools. This continued for a while until he started passing green, watery stools. Luckily, he had some Revive isotonic drink and lemonade in the fridge. He tried to rehydrate himself but eventually had to visit a 24-hour GP clinic for an injection, IV drip, and several hours of observation. He went home with two types of antidiarrheals, an anti-vomiting medication, a gastric medicine, and charcoal tablets. After taking a few days off to recover at home, he eventually made an uneventful recovery.
Figure 2: The basic principle in managing food poisoning is rehydration – when things get too bad, patients are given intravenous fluids to promptly replenish lost fluids and electrolytes (image courtesy of the benessair.com website).
Sze Ying, a college student, was awakened in the middle of the night with severe abdominal pain. She felt nauseous and started vomiting a curdy, yellowish substance into the bathroom sink. Within a few minutes, she began to break out in cold sweat, shiver, and feel her limbs grow cold. She tried to take two tablets of Paracetamol and drank a glass of warm water, but that did not help. She became extremely ill and asked her housemate to take her to the nearest emergency department or clinic. The on-call doctor attended to her, connected her to IV fluids, administered a range of IV medications, and within five minutes, she felt normal again. When asked by the attending consultant, Sze Ying recalled having had a glass of cold milk from the fridge an hour before she went to bed. She was sure the milk was not expired, but she remembered that the taste was a bit off. Thinking it was probably still safe to drink, she finished the whole glass and went to sleep. The attending physician explained that this was most likely the cause of her symptoms. Sze Ying was admitted overnight for observation and discharged the following day after regaining her appetite.

Figure 3: One of the common indicators that a food is no longer safe for consumption is that it has exceeded its expiration date, or when the food smells funny, even way before its expiration date – it all depends on how the food is stored (image courtesy of the Food and Home website).
Afiq, an out-of-towner, was in Penang for vacation with his wife. They had enjoyed themselves immensely in the old town, taking in the sights and the local food. Two days before they were due to return to KL, Afiq decided to wake up early and walk to a nearby morning market to have breakfast. Minutes into window-shopping at the various food stalls, he was greeted by a coffee shop with tons of customers seated around, sipping hot coffee and eating the local kaya and peanut butter bread. He soon came to learn that there is such a thing as roti kahwin, and ordered a couple of toasts for himself along with a cup of super-strong coffee. The food got the better of him, and he ended up drinking three full cups of the local coffee and licking the plate clean of all the delicious kaya. Proud of his find, he walked back to his hotel and gave it little thought. But then, disaster struck at the other end of his digestive tract, when three hours later, he started making regular visits to the toilet and passed out a large volume of yellowish stools that were initially mushy and subsequently watery. There was no stopping it, and if he could calculate the amount of time, he’d say more than 30 times. His legs were weak by the time he hit twenty times, and he started feeling feverish and nauseated. He couldn’t even drink and was so parched that his wife had to wring a towel dipped in cold water to cool him down. There was no way he could be transported to a nearby clinic, so an ambulance was called, and he was brought to the emergency department. Afiq was admitted for rehydration with IV drip, put on various antidiarrheals, Paracetamol, and a standard dose of probiotics. Thankfully, his recovery was swift as he came in early and was discharged three days later without complications. He has since sworn off the super-strong coffee. Upon recalling the events, he noticed a lot of flies in the stall and that the coffee tasted funny, but he drank it anyway since there were many other customers present. He was sure it would be okay, since the stall attracted so many loyal customers.

Figure 4: Always go with your gut feeling rather than following the crowd. Look around for telltale signs of unhygienic practices, the best of which is the Food Premises Grading certificate in Malaysia. Eateries are assigned grades based on the marks obtained through random inspections conducted by the local municipal council, with an A being the highest grade. Outlets with a D grade are often ordered to shut down (image courtesy of the iStockphoto.com website).

Figure 5: A buffet spread is the most convenient method to serve a large group of people in one setting. As easy as it may be, if food safety standards are not maintained, it can quickly turn disastrous. A quick search on the cdc.gov website will show you the number of cruises afflicted with outbreaks that are sometimes challenging to identify the pathogen (image courtesy of thedailymeal.com website).
Nathan, in his early sixties, was in a neighbouring country for work. He was enjoying the buffet spread in front of him during breakfast and selected a hearty assortment of cold cuts, omelettes, green salad, Chinese noodles, dim sum, and a plate of nasi lemak. After breakfast, he made his way to the hotel’s ballroom for a work-related meeting. Sitting through the usual drone of discussion, he was almost dozing off when he began feeling queasy in the upper stomach. He suspected it was the eggs he had earlier, and didn’t pay it much attention. He tried to drink some water to feel better, but within minutes, he broke out in sweats and vomited all over the floor. The delegates nearby were attentive and helped send him to the sick bay. Hours later, his condition worsened as he vomited more and more and began passing large volumes of green stools. He was advised to go to the hospital, but he remained stable enough to decline, stating he wanted to fly back to Malaysia. This was a show of bravado, but soon after he landed in Penang, he had to be taken to the emergency department by an ambulance. He was in shock, with comorbidities including hypertension, diabetes, and stable heart disease. Preliminary blood tests revealed acute kidney injury, electrolyte imbalance, concentrated urine, abnormal liver enzymes, an elevated infective panel, and low blood sugar. The attending doctors managed to resuscitate him with fluids and started him on IV antibiotics, along with other standard IV medications. He was admitted to the intensive care unit for close monitoring. Over the next 24-48 hours, he gradually recovered without complications and was transferred to the regular ward. Blood cultures and stool analysis confirmed the presence of Escherichia coli, and his antibiotics were adjusted accordingly to match the sensitivity results.
Now that we have all witnessed the common clinical scenarios of food poisoning, let us delve into the topic.
Food poisoning, also known as foodborne illness, is an illness caused by eating contaminated, spoiled, or toxic food. While most cases are mild and resolve without treatment, food poisoning can sometimes be severe and even life-threatening, especially for vulnerable groups like young children, older adults, pregnant individuals, and those with weakened immune systems.
Food poisoning is typically caused by bacteria, viruses, parasites, or toxins that are present in food. Contamination can occur at any stage, including during production, processing, storage, or preparation.
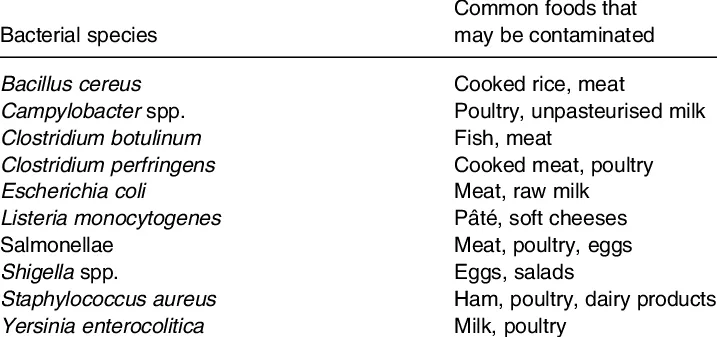
Figure 6: Although the bacterial cause for food poisoning varies extensively, the treatment principles stay the same – to rehydrate, to replenish both fluids and electrolytes, to stop vomiting and diarrhea, and lately, to counter the pathogenic effect of the toxins with probiotics. Antibiotics are only administered to a select group of high-risk patients (image courtesy of Gibson GR et al., British Journal of Nutrition, 2005).

Figure 7: An image illustration of common symptoms of food poisoning (image courtesy of the russellworthsolicitors.co.uk website).
Symptoms can begin within hours or even days after consuming contaminated food. The severity and type of symptoms depend on the cause, but typically include:
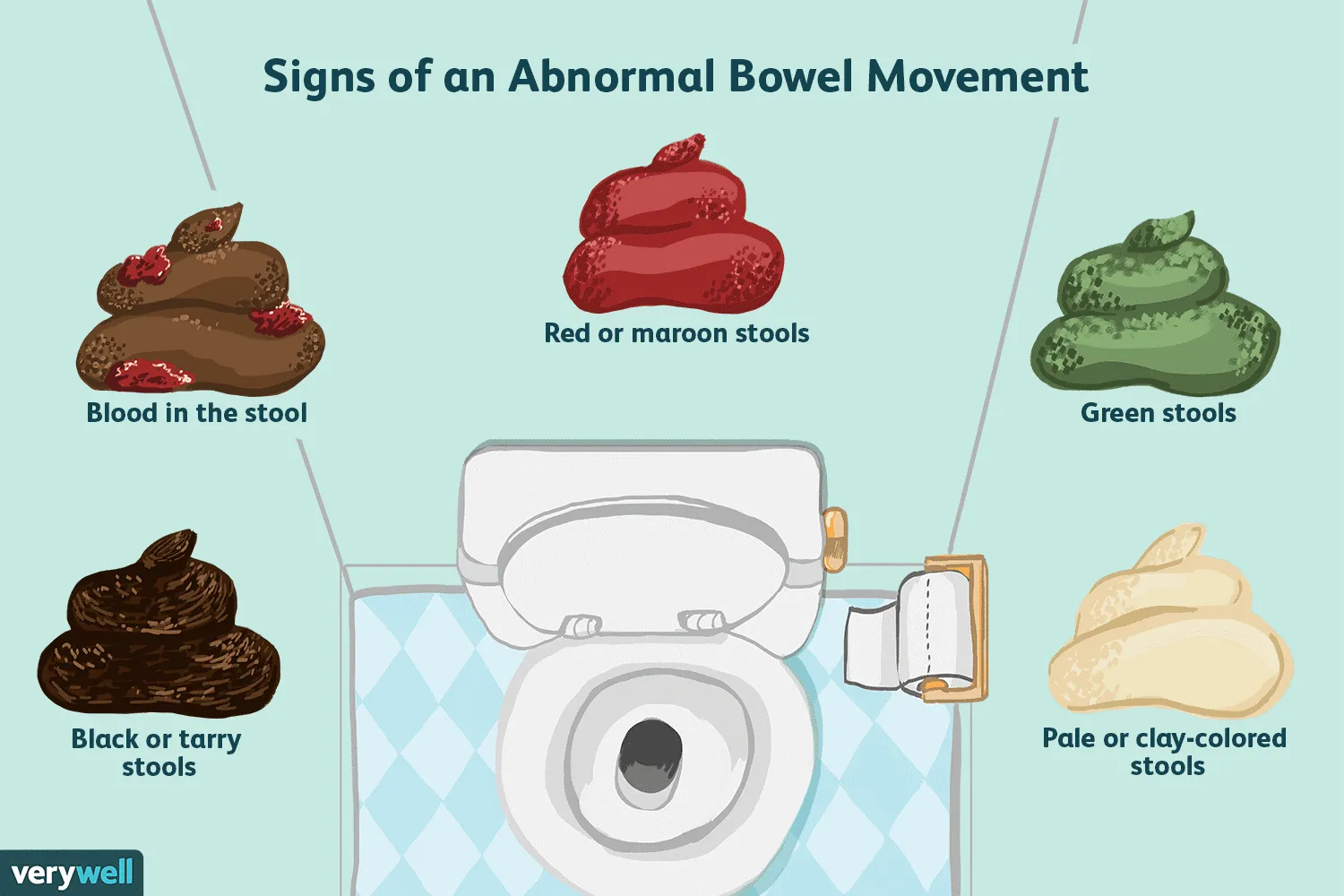
Figure 8: Help your doctor by not only documenting the frequency of your diarrhea, but also the texture, the volume, and most importantly, the colour of your stool. Although the colour of your stool could be influenced by the type of food you eat, accompanied by food poisoning symptoms, it usually suggests an underlying bacterial or viral infection, e.g., salmonellosis, shigellosis, giardiasis, Rotavirus, or Norovirus (image courtesy of the verywellhealth.com website).
In severe cases, food poisoning can lead to dehydration, kidney failure, neurological symptoms, or even death.

Figure 9: High-risk groups are those who are aged 65 or older, children under 5, pregnant women, and people with weakened immune systems (patients receiving chemotherapy, immunosuppressants such as steroids, those on immunomodulators, groups afflicted with diabetes, liver disease, kidney ailments and/or on hemodialysis, chronic alcoholism, HIV infection, autoimmune disorders, or cancers) (image courtesy of the cdc.gov website).
These groups are more likely to suffer from severe symptoms and complications.
Most cases of food poisoning resolve on their own without the need for medical intervention. However, severe symptoms or prolonged illness may necessitate medical attention.
Doctors usually diagnose food poisoning based on symptoms and a history of what was recently eaten. In some cases, stool, blood, or food tests may help identify the pathogen.
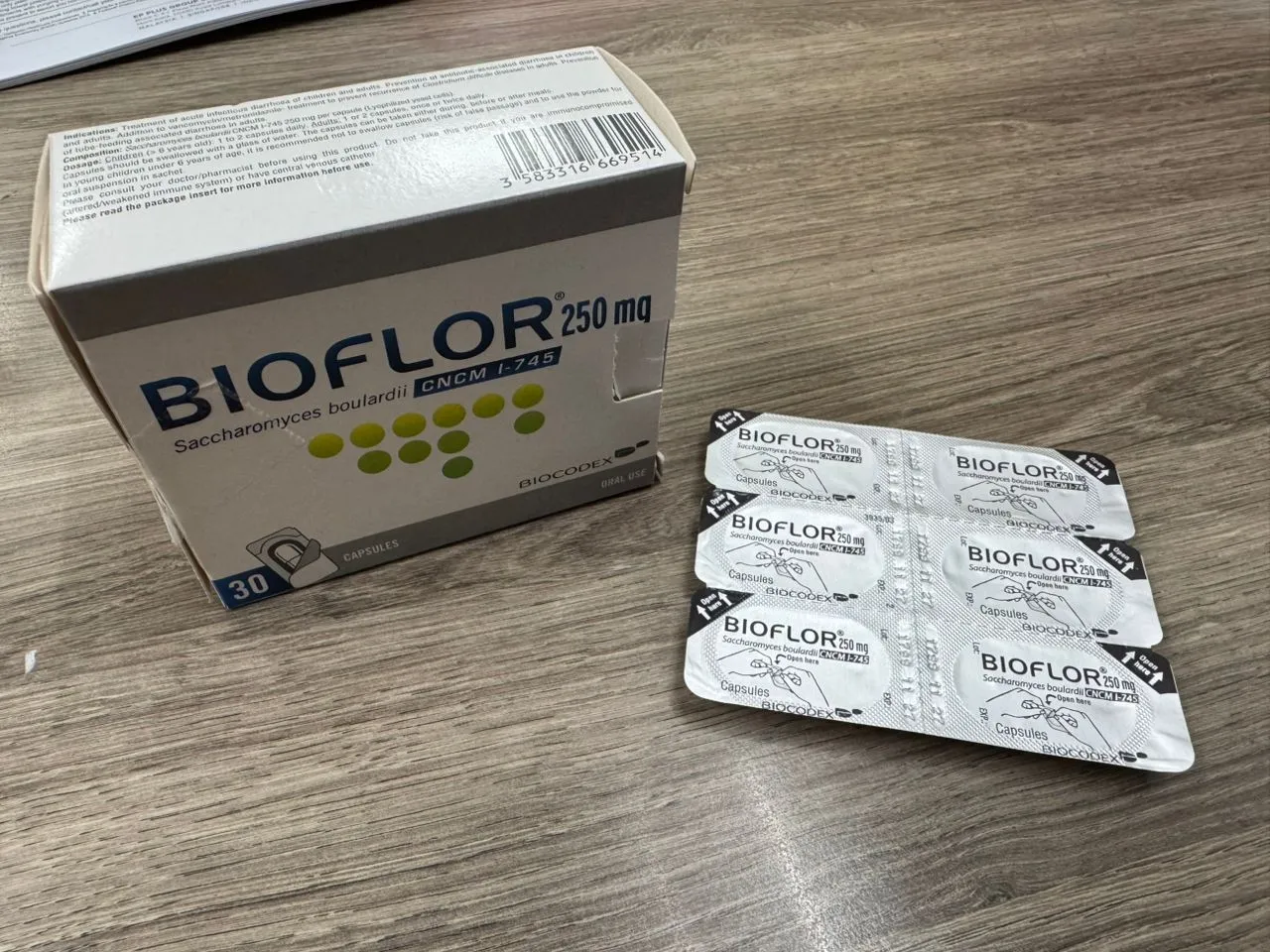
Figure 10: When taken within 48 to 72 hours of symptom onset, this fungal-based probiotic can shorten the duration of infection, reduce symptom intensity, and protect the local gut microbiome.
Seek prompt medical help if you experience:
Young children, older adults, pregnant individuals, and those with underlying health conditions should exercise caution.
The best way to avoid food poisoning is by practising proper food safety from the market to the table.
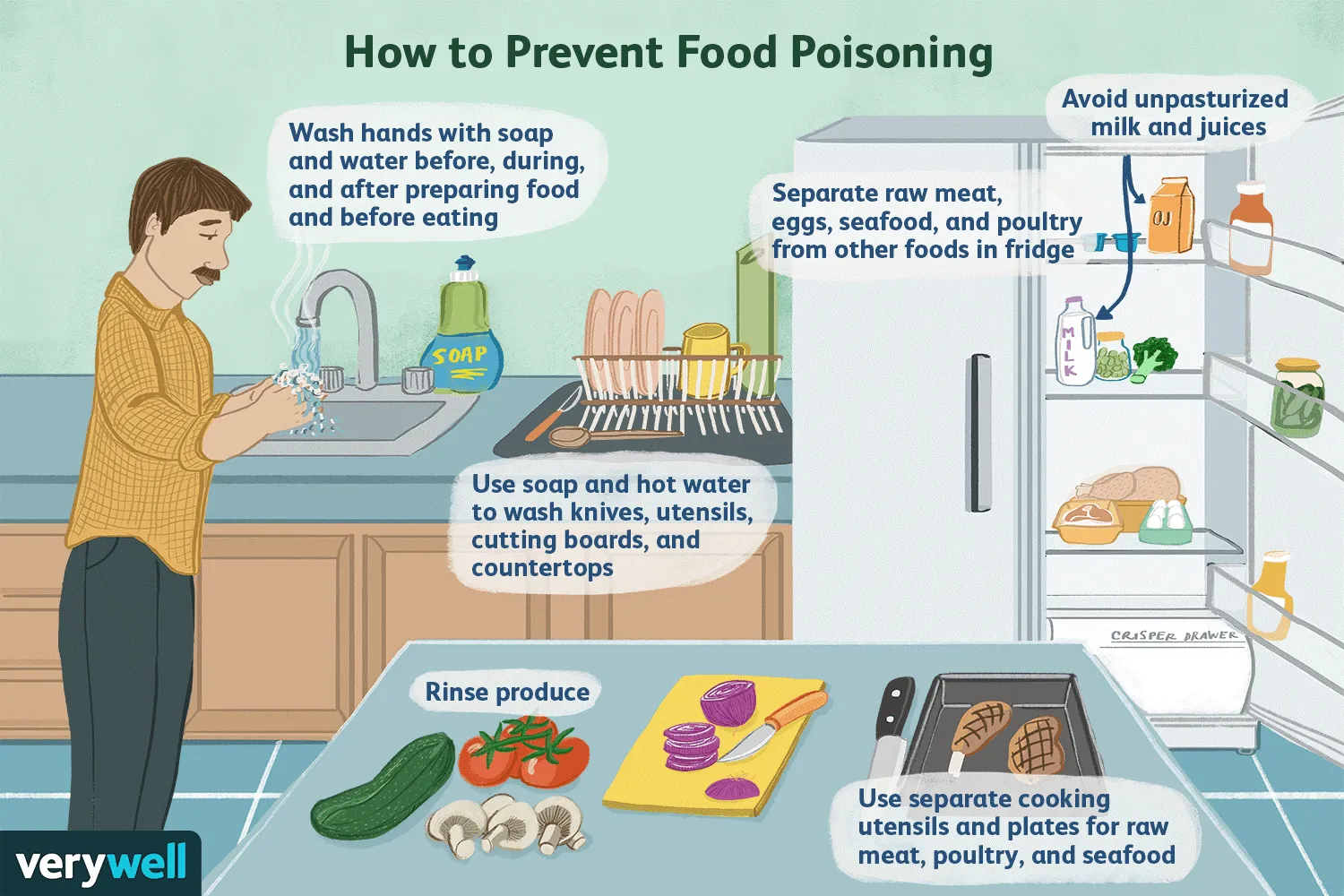
Figure 11: A cartoon illustration of best practices to prevent food poisoning (image courtesy of the verywellhealth.com website).

Figure 12: A simple guide to gauge the food safety standard for a food premise is to look out for such certificates displayed on the walls inside the restaurant (image courtesy of the Majlis Bandaraya Seberang Perai website).
Although most people recover completely, food poisoning may occasionally cause complications:
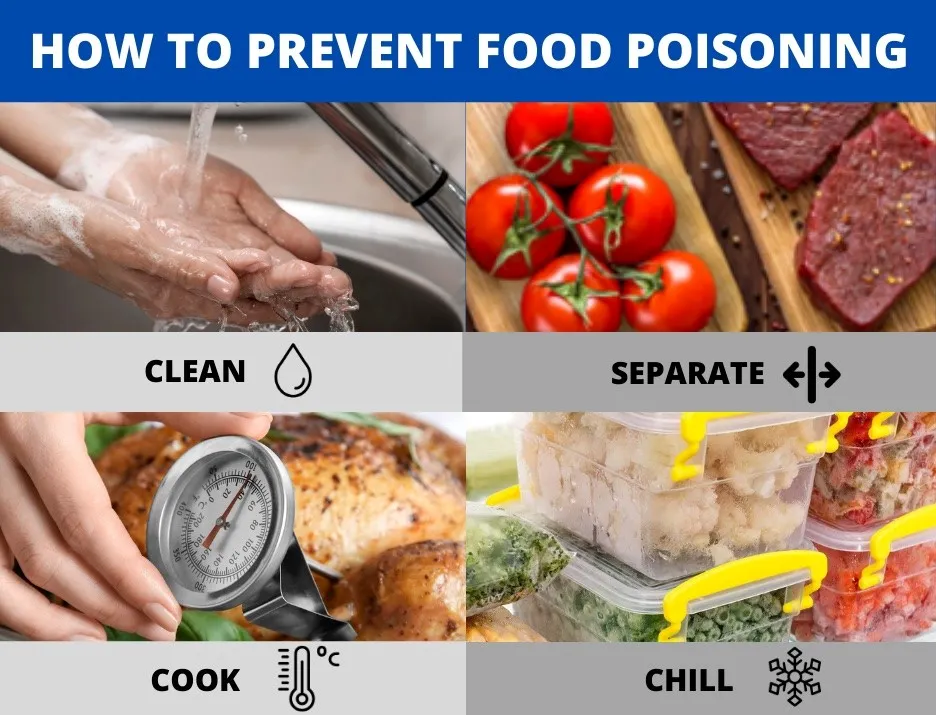
Figure 13: The take-home message on food safety from today’s article – clean your hands, separate cooked and uncooked food, cook your food thoroughly, chill and store excess food safely (image courtesy of the ISO 22000 Malaysia website).
Food poisoning is a common but preventable health problem. By understanding its causes, recognising symptoms early, and practising safe food handling and preparation, individuals can protect themselves and their loved ones. Although most cases of food poisoning are mild, it is important to take them seriously, especially for those at higher risk. When unsure, always seek medical advice. Staying alert and informed is essential for eating safely—turning meals from a source of worry into a source of comfort.