INTRODUCTION
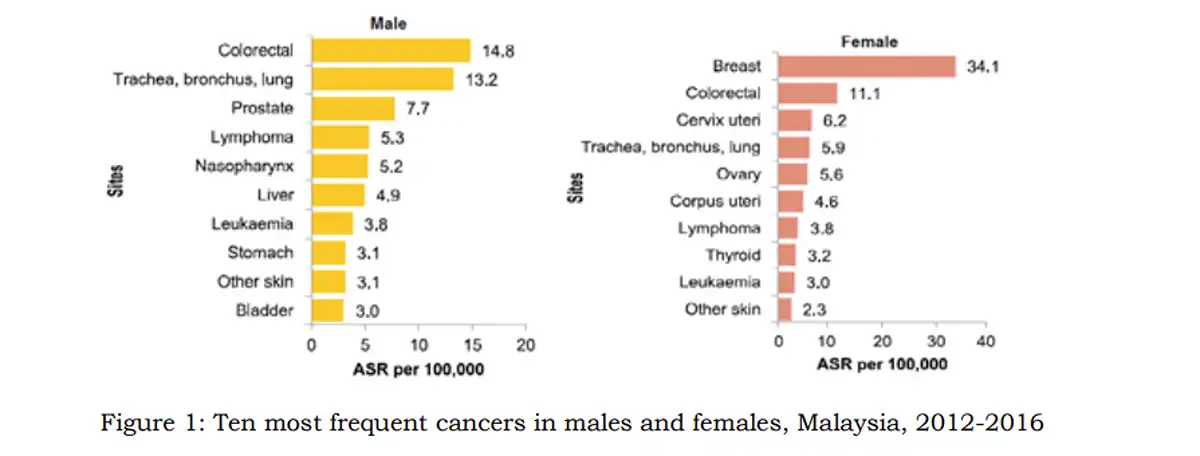
Figure 1: Top ten cancers in Malaysia based on genders
Colorectal cancer is the third most common cancer worldwide, accounting for 10% of all cancer cases. It is also the second leading cause of cancer-related deaths globally. In Malaysia, colorectal cancer is the second most frequently diagnosed cancer, representing an alarming 13.5% of all new cancer cases reported from 2012 to 2016. The incidence of this disease is higher in males than in females. Risk factors for developing colorectal cancer include being over 50 years of age, lifestyle choices such as smoking, excessive alcohol consumption, obesity, a sedentary lifestyle, high intake of processed foods and red meats, and a low intake of fruits, fiber, and vegetables.
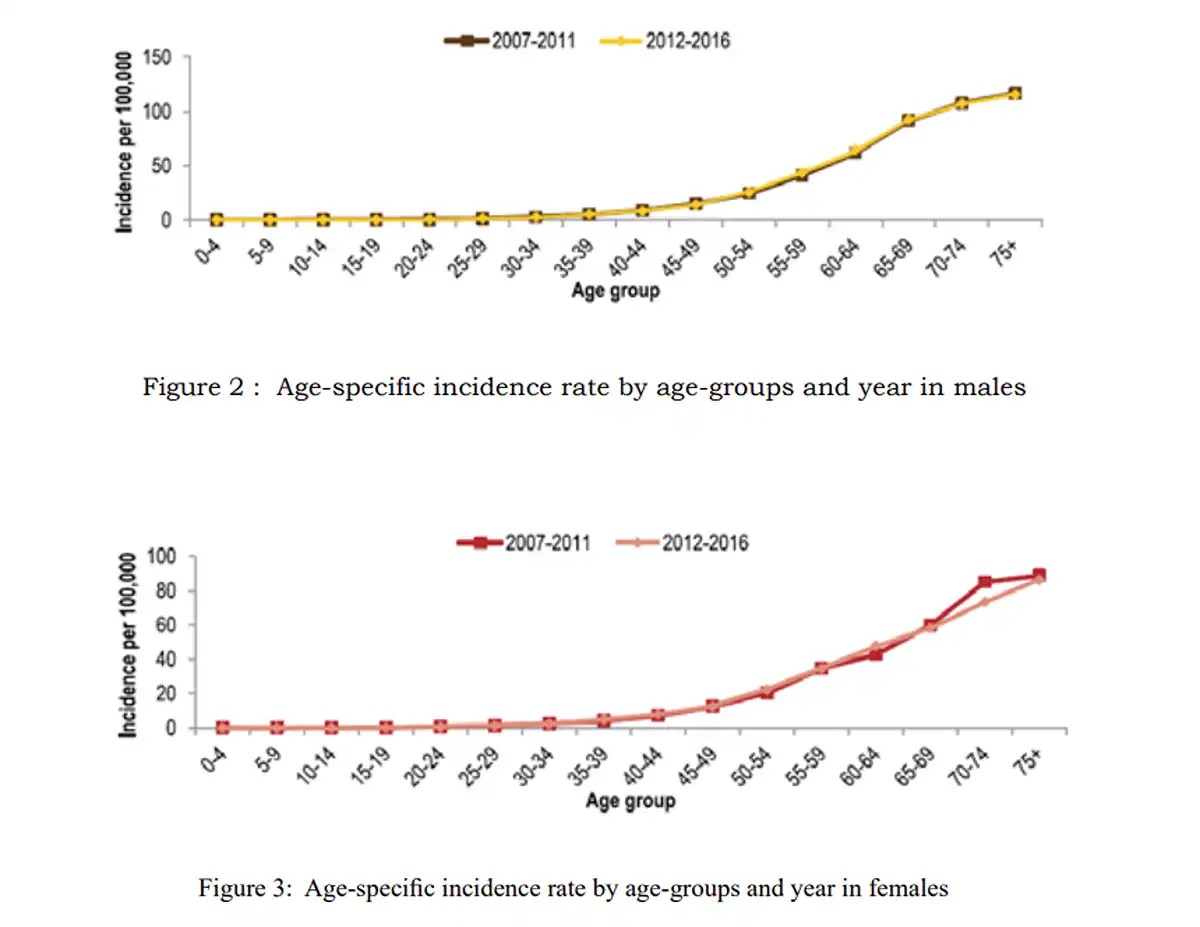
Figure 2: Incremental risks of colorectal cancer incidence according to age
DIAGNOSIS AND SCREENING
Diagnosing colorectal cancer often occurs late, with many cases being detected at advanced stages where curative treatment becomes difficult, if not impossible. This late diagnosis can have severe consequences, significantly impacting life expectancy. The reason for this delay is that early-stage cancers typically do not exhibit symptoms due to their small size. Consequently, it is essential for patients to be aware of colorectal cancer and to utilize early screening tools, such as stool occult blood tests and colonoscopies. These tests aim to detect cancer early and identify polyps—benign or pre-cancerous growths—when they are still small. When identified, these polyps can often be removed endoscopically.
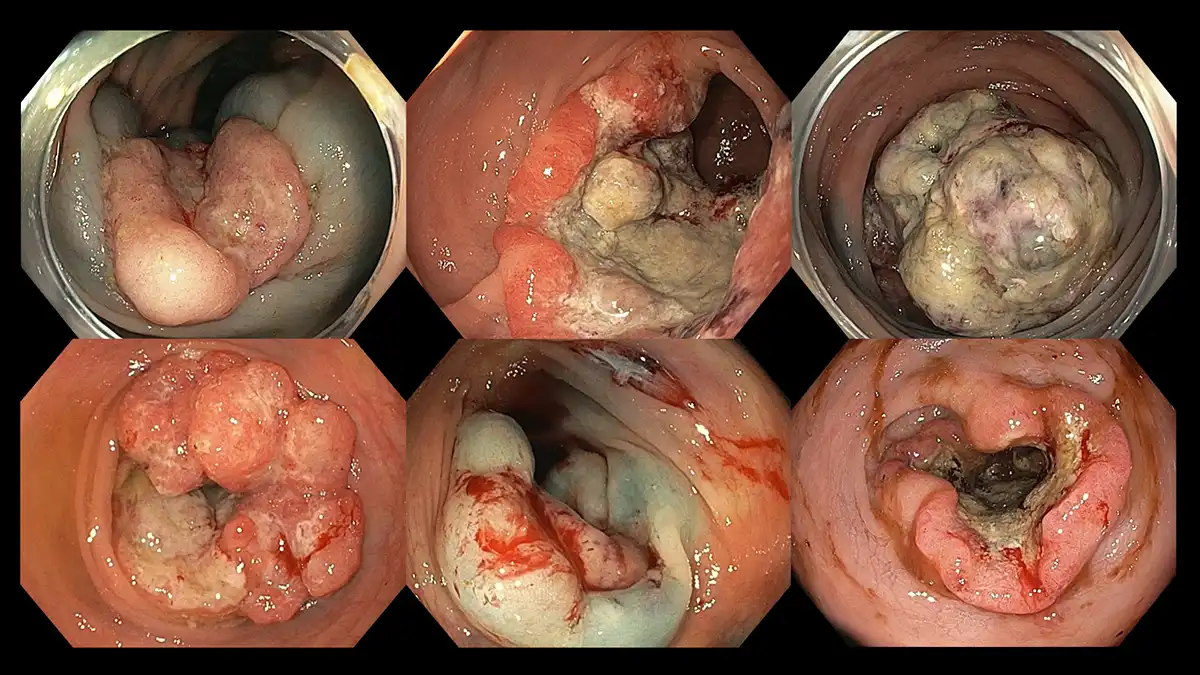
Figure 3: Various morphology of advanced colorectal cancer – fungating, ulcerative, and polypoidal
Fortunately, more than 90% of these polyps are small (less than 1 cm) and can be removed simultaneously during the colonoscopy by using a thin wire snare. Larger and more complex polyps, if detected early, may still be removed endoscopically in tertiary centers with expertise in advanced techniques such as endoscopic mucosal resection, endoscopic submucosal dissection, and full-thickness resection. However, invasive cancers often become friable and can lead to bleeding and mechanical obstruction, resulting in symptoms like lower gastrointestinal bleeding, constipation, changes in bowel habits, long-term loose stools, appetite loss, involuntary weight loss, ongoing abdominal discomfort, and a sensation of incomplete evacuation after defecation. By the time these symptoms appear, the likelihood of successfully removing polyps endoscopically decreases, as this treatment may not adequately cure the disease.

Figure 4: Progression interval of colorectal polyps to advanced cancers
All colorectal cancers originate from small polyps, and achieving curative intent involves completely removing them before they exhibit malignant features. Polyps take time to develop, typically growing larger or invading deeper intestinal layers over a period of approximately 8 to 10 years. If we can interrupt this progression, the goal to prevent cancer is achieved.

Figure 5: Subtle colorectal polyps detected with high-definition colonoscopy and characterized with image-enhanced endoscopy
Thus, colonoscopy is an essential tool and a gold-standard diagnostic procedure for achieving these objectives. The recommended age to begin screening has been lowered to 45 years, with earlier screening advised for individuals with specific risk factors, such as a positive family history of colorectal cancer, hereditary or genetic conditions, and/or inflammatory bowel disease.
STOOL OCCULT BLOOD TEST

Figure 6: Home stool occult blood test kit
That said, we recognize that some patients may feel uncomfortable with undergoing a colonoscopy. For this group, a non-invasive option is the stool occult blood test. These test kits are easy to use and can be conducted annually. The test operates on the principle that polyps can bleed when stool comes into contact, leading to micro-bleeding that is not visible to the naked eye. These kits can detect such occult blood. If the result is positive, patients are then referred for further evaluation and possibly completing the assessment with a colonoscopy. However, it’s important to note that these kits are not foolproof. Small, subtle, and flat polyps might be missed, necessitating more frequent testing intervals. Additionally, for patients with a known history of lower gastrointestinal bleeding from conditions such as anal fissures, hemorrhoids, rectal ulcers, inflammatory bowel disease, or diverticular disease, the stool test kits may not truly identify the source of bleeding arising from polyps.
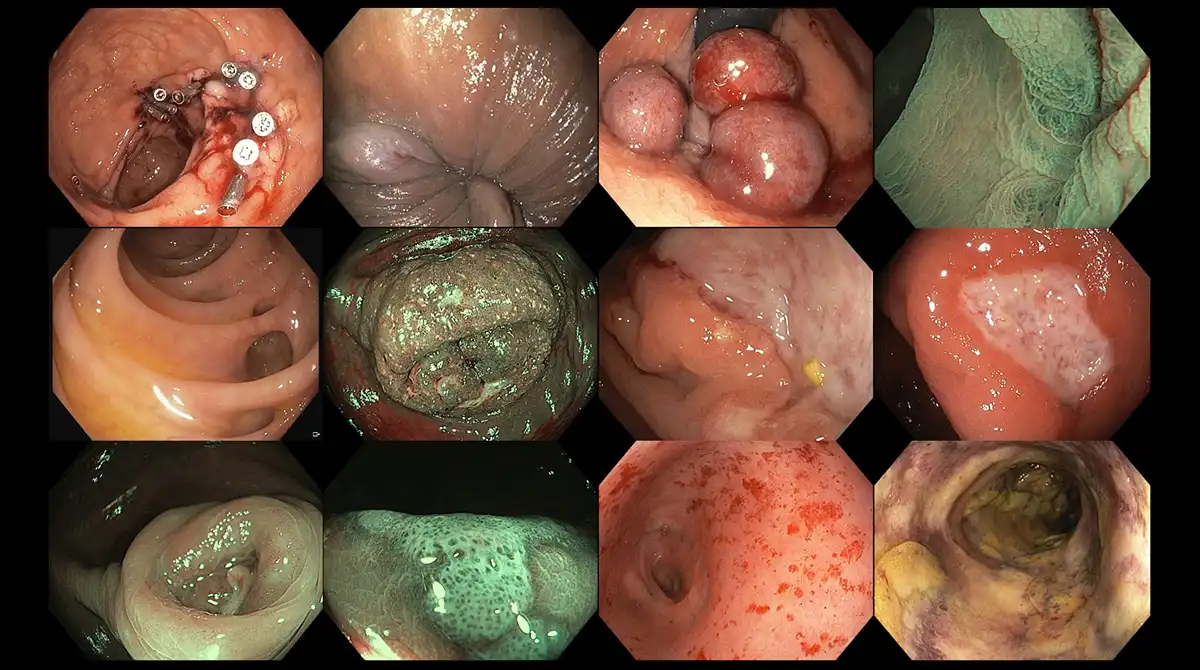
Figure 7: Various non-malignant causes for false positives in stool occult blood test kits – colon and rectal ulcers, anal fissures, internal haemorrhoids, diverticular diseases, colonic inflammation, appendiceal inflammation, solitary rectal ulcer syndrome, rectal inflammation from previous radiotherapy, inflammatory bowel diseases
COLONOSCOPY

Figure 8: Latest and most modern colonoscope from Olympus
Colonoscopy is a minimally invasive procedure which is highly effective in detecting and removing colorectal polyps. The colonoscope is a long, flexible tube equipped with a powerful light source at the tip. It has a diameter of 13.2 mm, which is larger than that of a traditional gastroscope (9.9 mm). Diagnostic endoscopic procedures are typically performed as day care procedures, and patients are assured that conscious or twilight sedation will be provided, which is generally sufficient for pain and discomfort during the colonoscopy. The procedure usually lasts anywhere between 15 to 20 minutes, though it may take longer if larger or more complex polyps are identified.
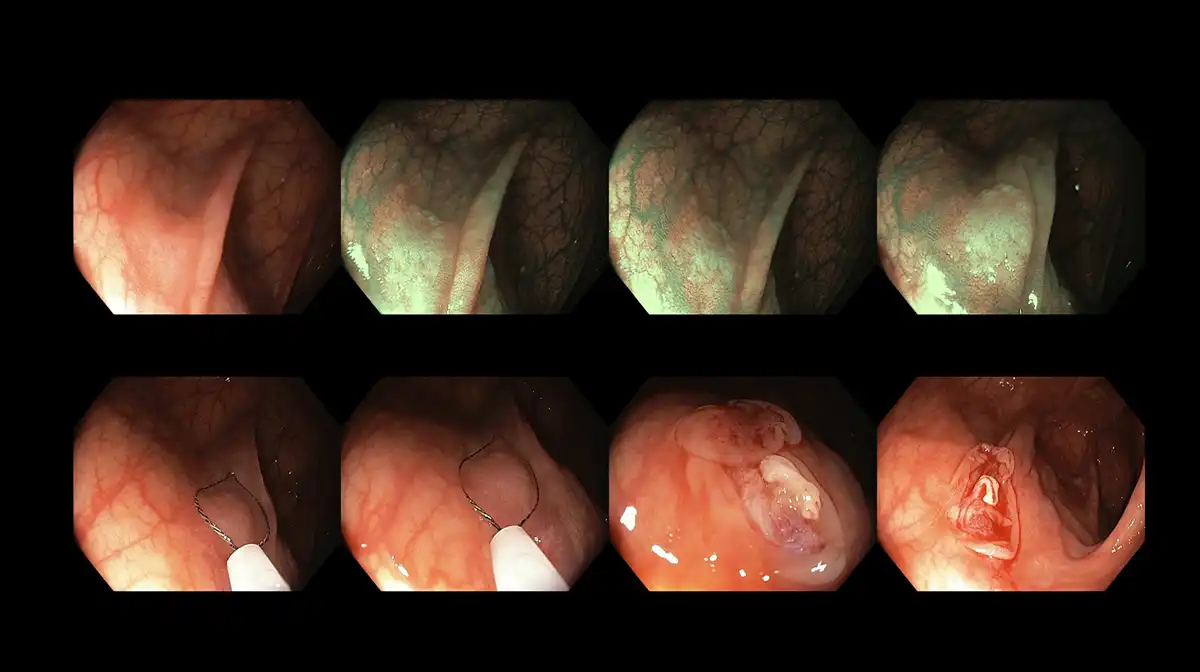
Figure 9: Conventional cold snare polypectomy to remove a subtle colonic polyp
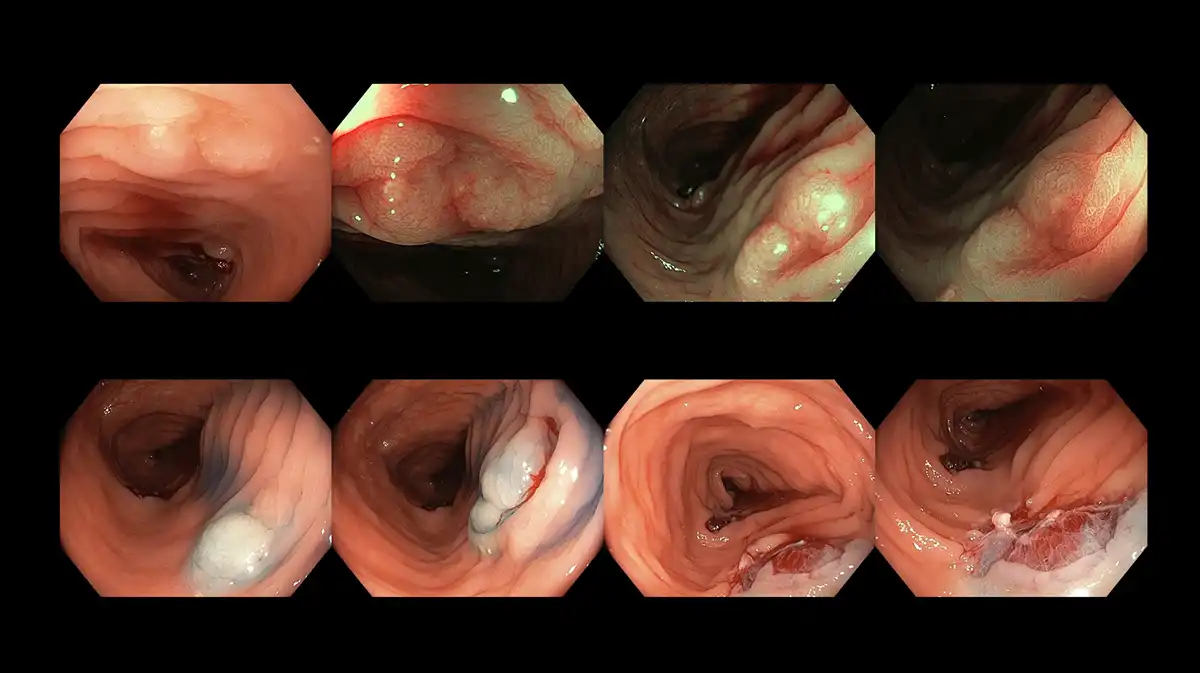
Figure 10: Piecemeal cold snare endoscopic mucosal resection to completely excise a polyp detected during colonoscopy
The trickiest aspect of colonoscopy is the preparation, during which patients are required to drink 3 to 4 liters of laxative (polyethylene glycol) the day before the procedure, over a period of 8 to 10 hours. Patients must manage not only the large volume of liquid but also its taste. The commercial laxative used, Fortrans, has a sweet flavor with a salty tang, making it relatively easy to drink if consumed slowly rather than rushed. Polyethylene glycol is safe for individuals who need to limit fluid intake (heart failure, kidney failure or liver impairment), as it is designed as a non-absorbable liquid. To improve compliance with the preparation, various strategies can be employed to ease this burden. Additionally, patients must follow a modified low-residue diet 1 to 2 days prior to the procedure. Foods to avoid include dairy and soy products, vegetables, fruits, oats, grains, and dark-colored liquids (red, purple, or black). Instead, patients are encouraged to consume plain, white foods such as porridge (broth), noodles, soup, chicken and fish (without skin), pasta, egg whites, and steamed buns. These dietary modifications help facilitate digestion and improve the outcome of bowel preparation, making it easier to achieve the desired results.
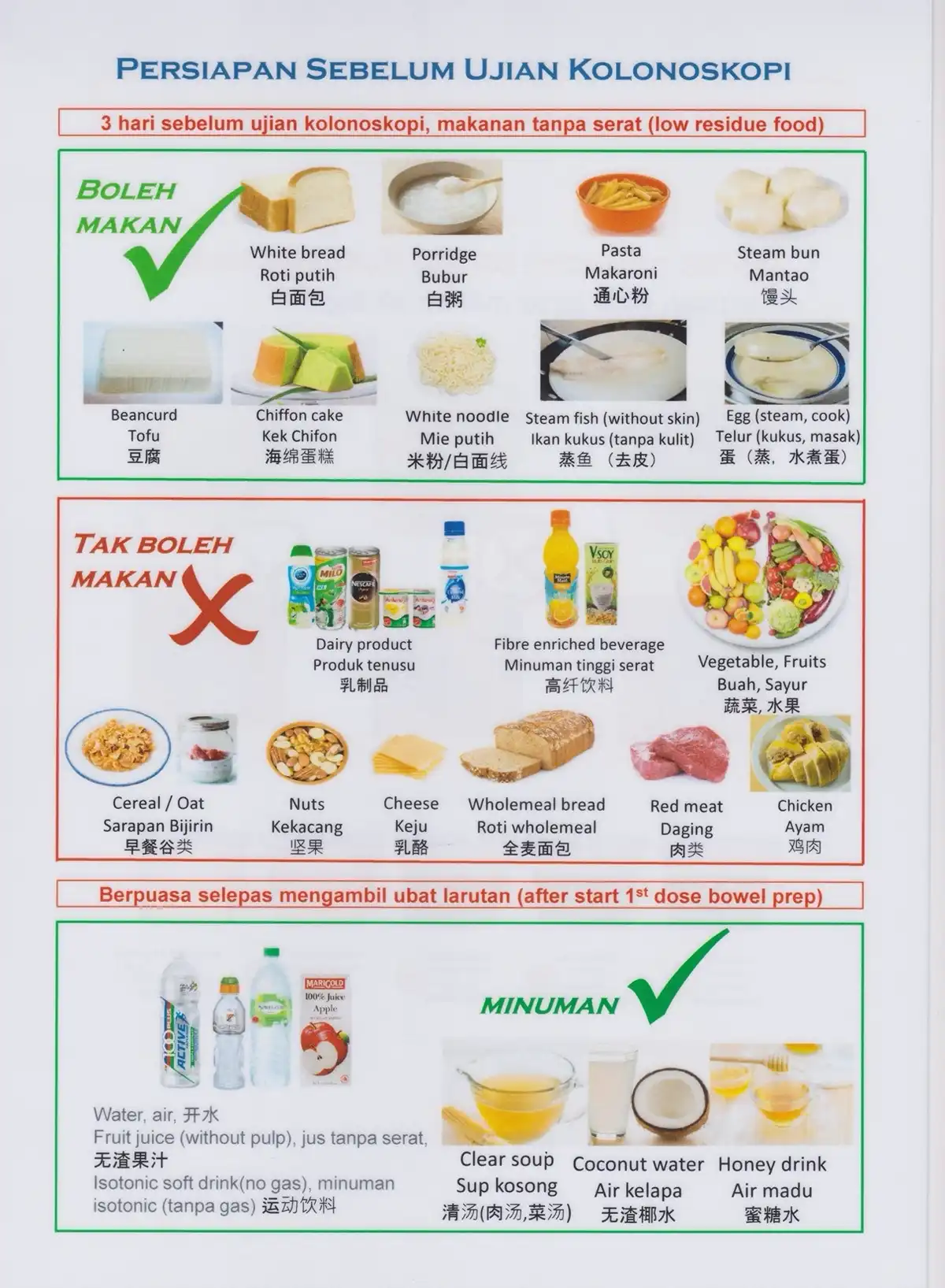
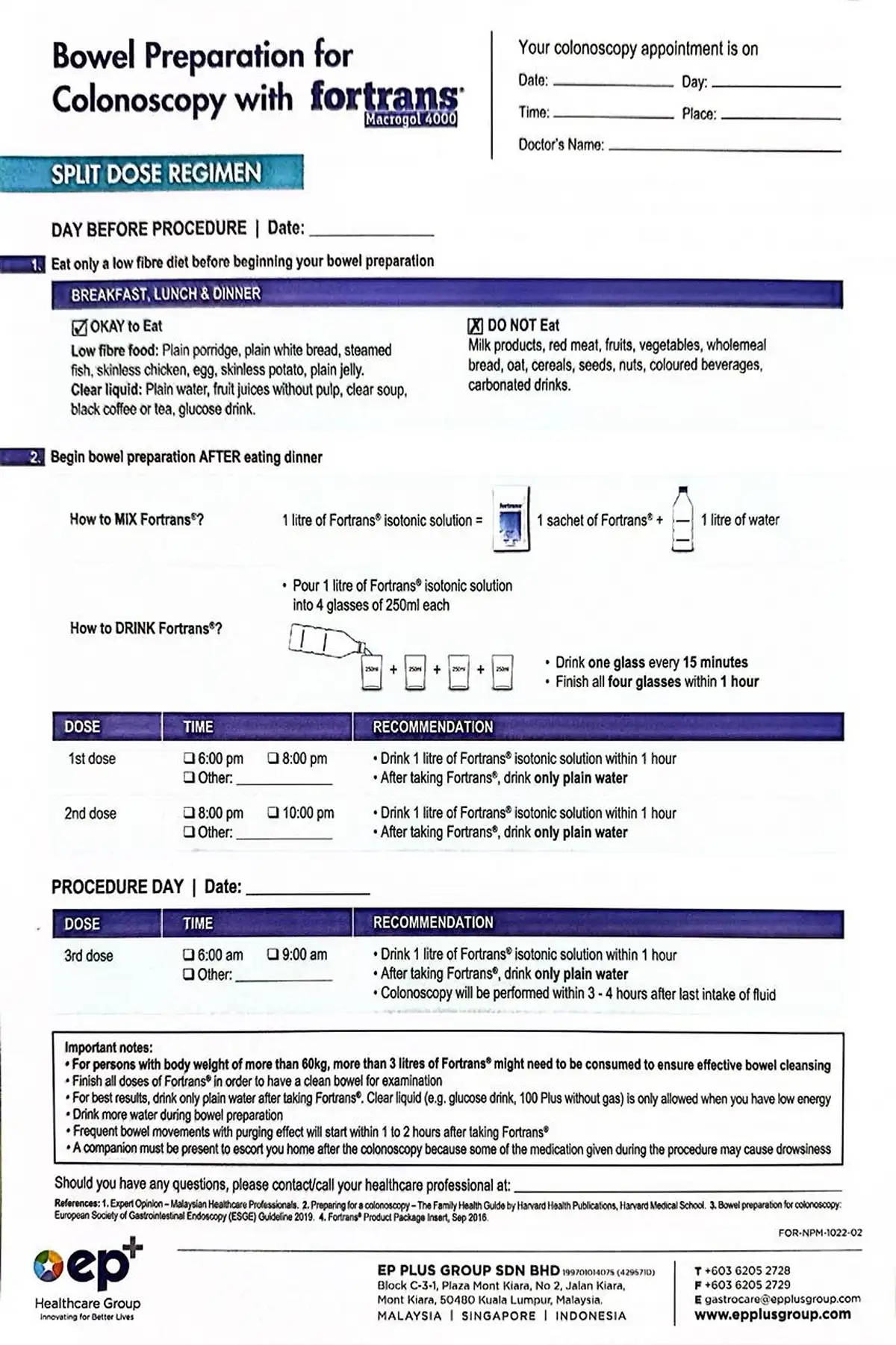
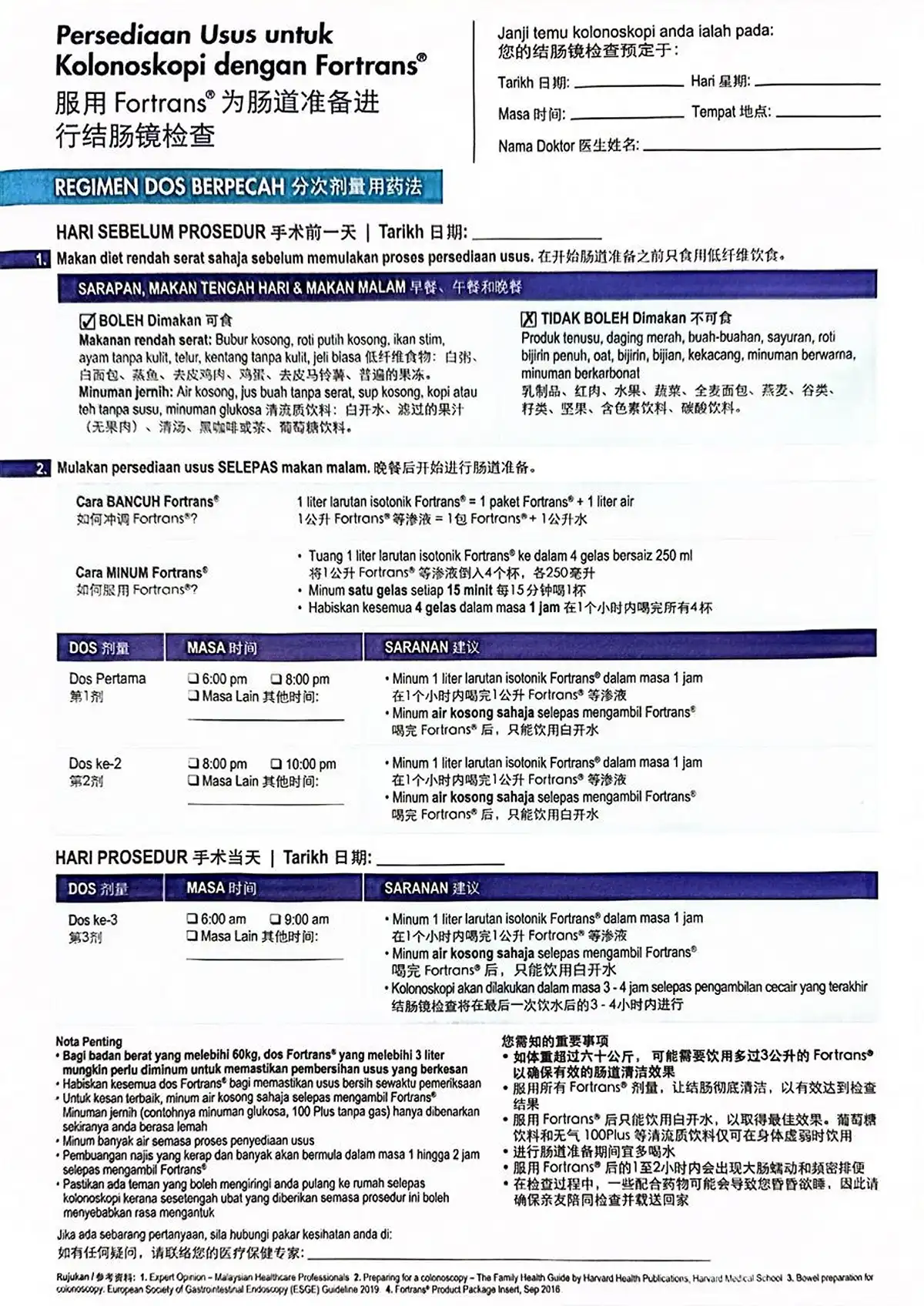

Figure 11: Bowel preparation instructional sheets for patients
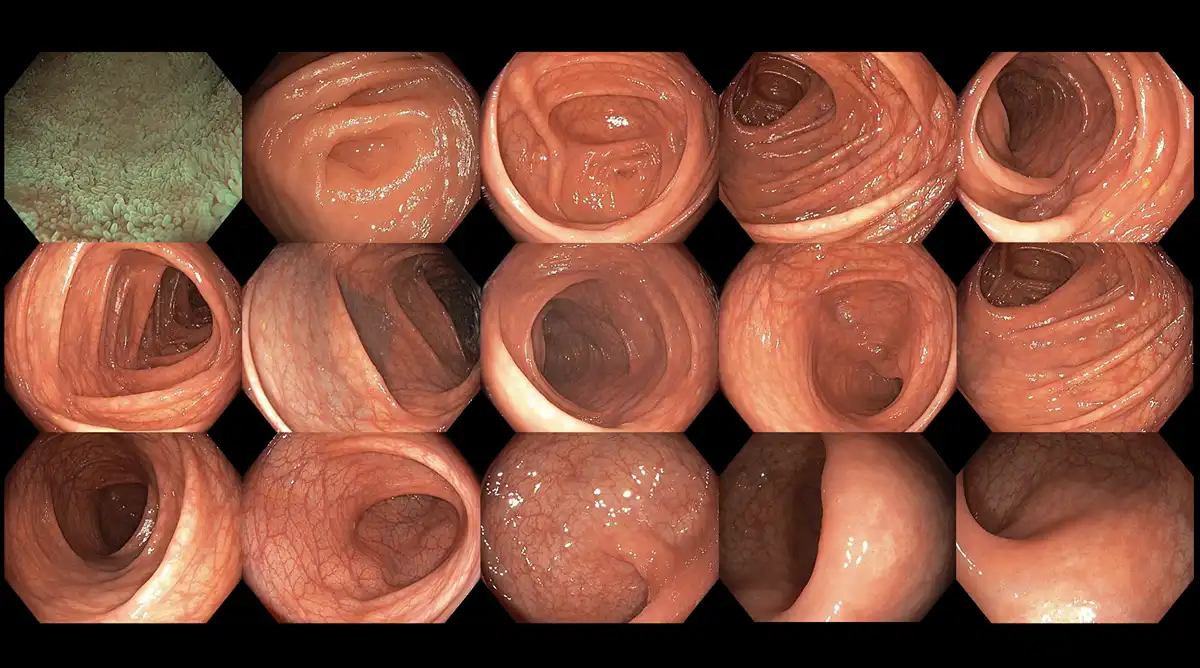
Figure 12: An example of an excellent bowel preparation during colonoscopy
Once patients have adhered to all the instructions and see clear effluent in the toilet bowl, they are ready for the colonoscopy. Nurses will position the patient on their left side, place an oxygen cannula at their nostrils, and administer intravenous sedatives. The doctor will then insert the tip of the colonoscope into the rectum and navigate it through the colon, reaching the cecum and sometimes even the terminal ileum of the small bowel. As the doctor withdraws the colonoscope, the inspection begins, with a focus on identifying polyps and other potential pathologies. Thanks to advanced optics and evolving endoscopic technology, doctors can now utilize image-enhanced endoscopy techniques, such as the Olympus narrow-band imaging (NBI) or the Fujinon intelligent chromoendoscopy (FICE), to examine the surface and lining of the bowels, distinguishing normal from abnormal tissues, characterizing identified polyps, and assessing their grade and invasiveness to guide biopsies and resection options. Photographs and videos may be taken to assist in the final report.
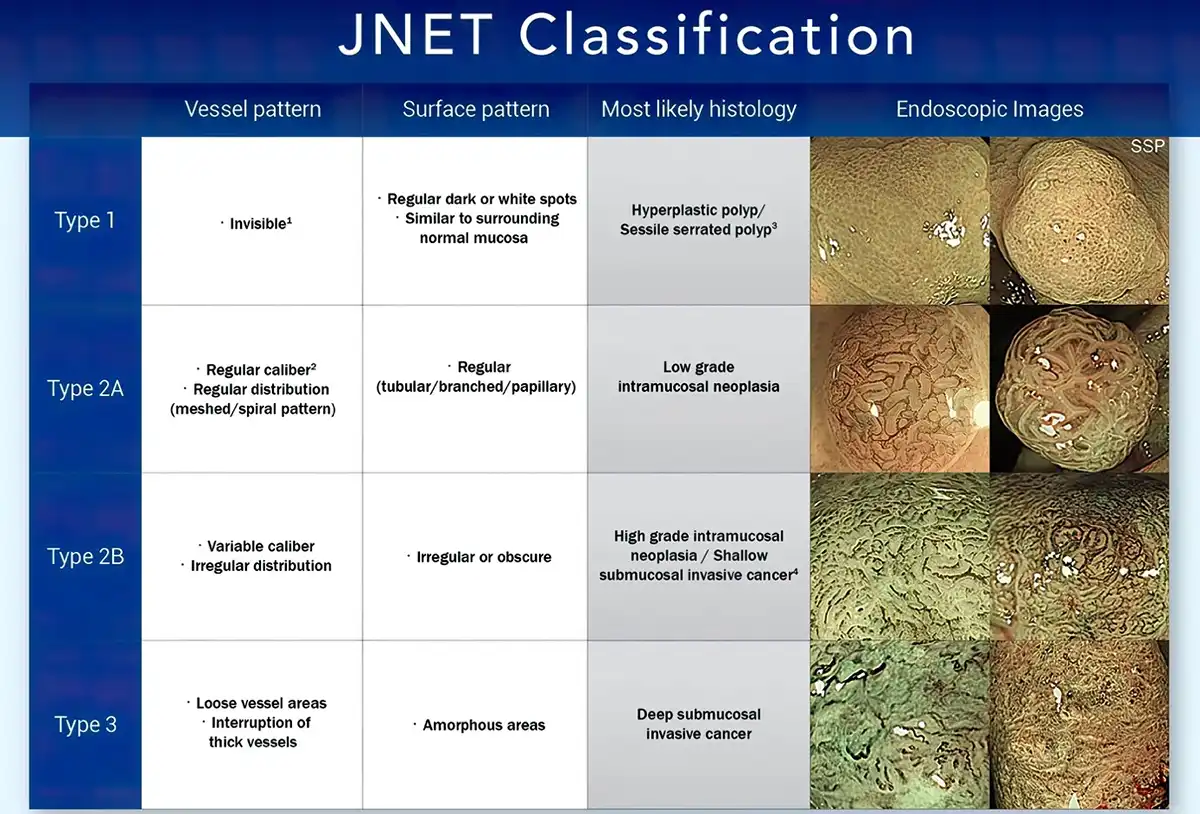
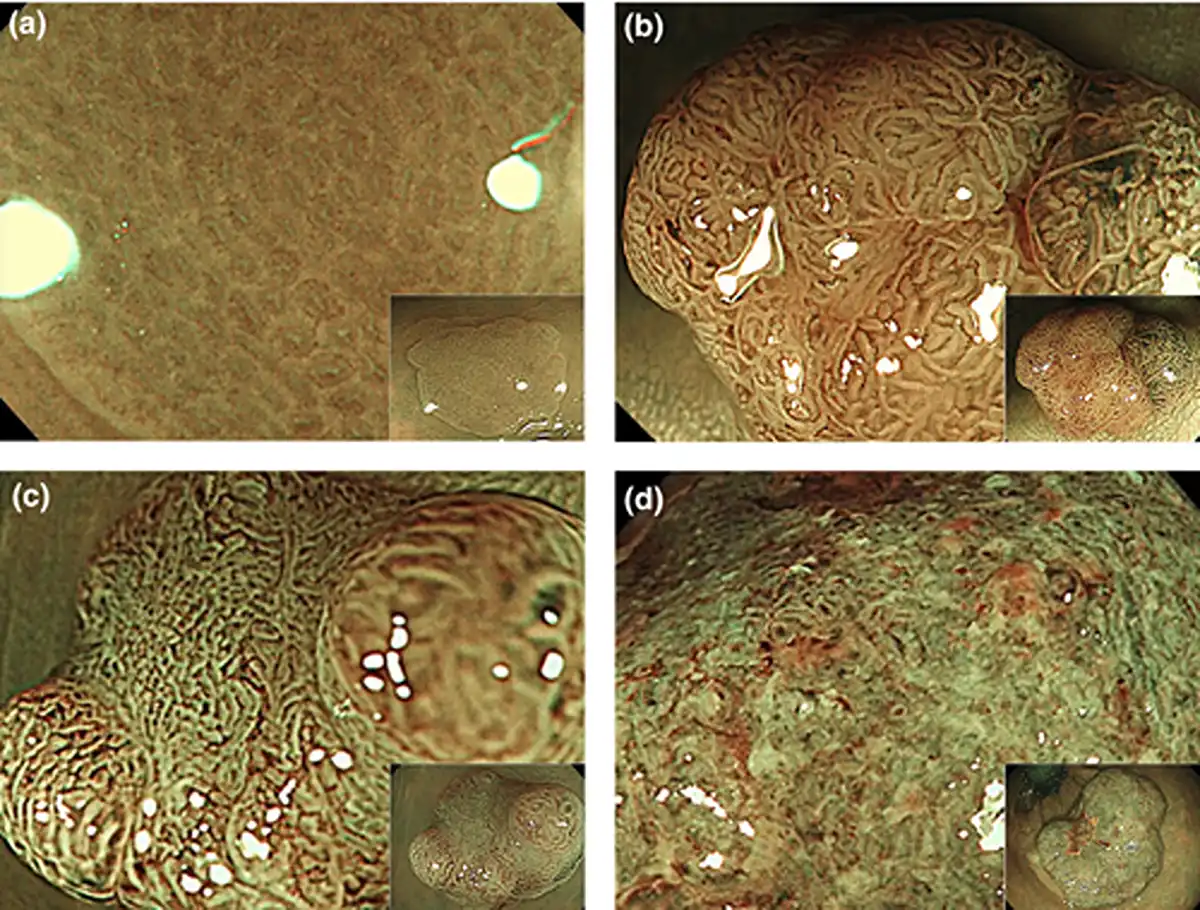
Figure 13: Standardized classification used for polyp characterization to ascertain the type of polyps along with discerning the grade and invasiveness to determine resection modalities
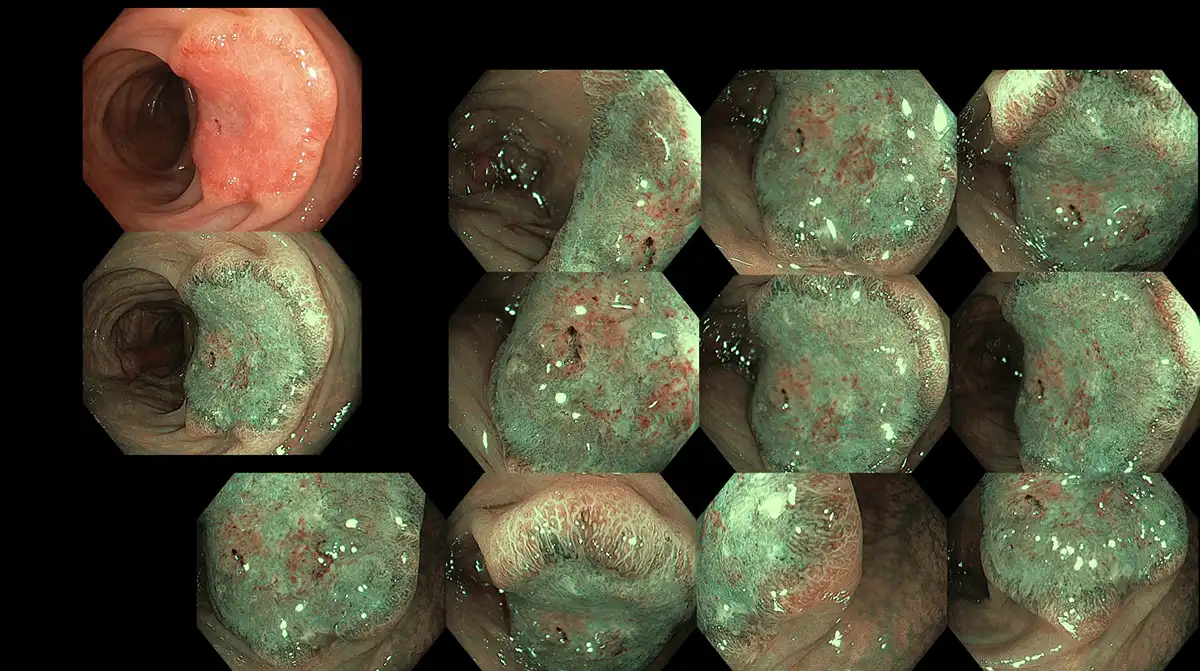
Figure 14: Polyp characterization of a deep invasive cancer with image-enhanced endoscopy using the Olympus narrow-band imaging technology
Patients can be reassured that they will remain comfortable throughout the procedure and will not retain any memory of it due to the type of sedatives used. Once the colonoscopy is completed, patients will be monitored in the endoscopy unit for up to 30 minutes, during which their blood pressure, heart rate, and oxygen saturation will be closely observed. Recovery time may vary; some patients regain full consciousness shortly after the procedure, while others may take an hour or two. Some bloating is normal as gases are used to distend the bowels for inspection. Many centers are now switching to carbon dioxide gas, which is reabsorbed faster than conventional oxygen, resulting in a more satisfactory experience for patients. Once fully awake, patients will receive a snack, and the doctor will discuss the colonoscopy results before they are discharged. A follow-up appointment will be scheduled to review any specimens collected or polyps removed.
Complications of colonoscopies and sedation are rare nowadays, but they generally include bleeding, perforation, aspiration, infection, and missed lesions. We would discuss these potential complications with the patients pre-procedurally, but reassure them that such complications are unlikely to occur in a diagnostic colonoscopy. With improved endoscopes and operating systems, in addition to better endoscopic accessories, bleeding and perforation complications, should they occur, can now be managed endoscopically.
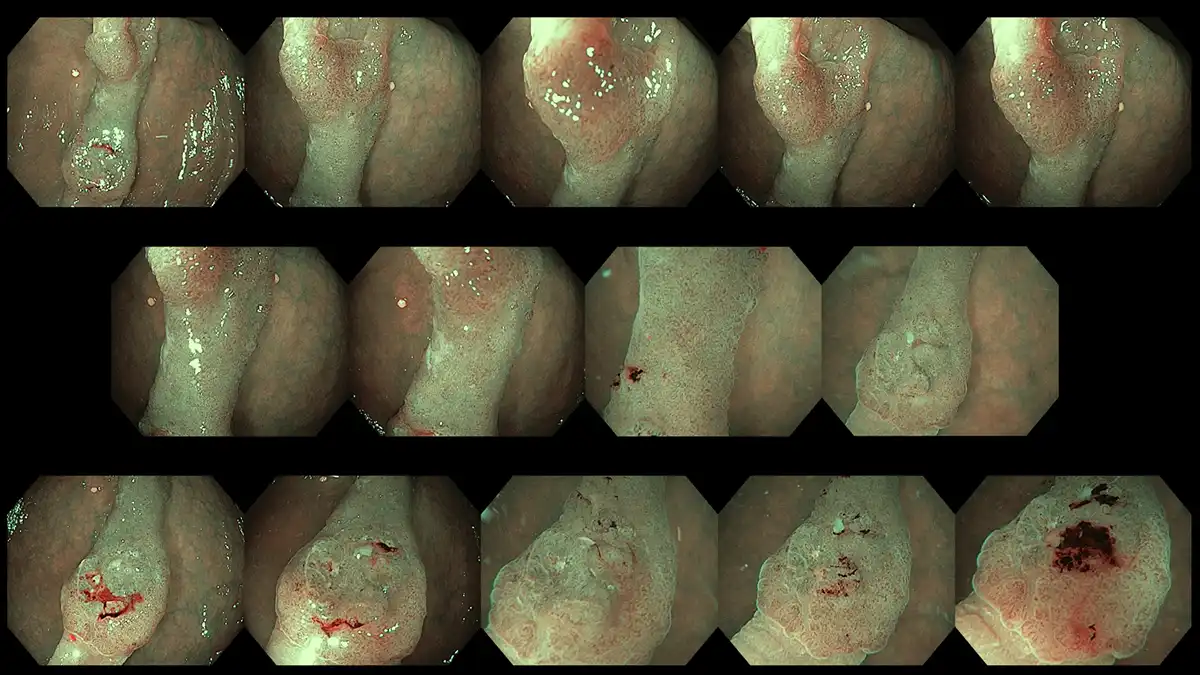
Figure 15: Another example of characterization of an intermediately sized polyp with deep invasion which is not amenable for endoscopic removal
CURRENT CHALLENGES
Despite strong evidence and emphasis on how early detection saves lives, 88% of the average-risk population in Malaysia has not undergone any form of colorectal cancer screening. Reasons for this include unawareness, indifference, fear of discomfort stemming from negative experiences shared by friends or relatives, unpleasant bowel preparation, inconvenience due to potential side effects, cultural beliefs and misconceptions, busy schedules, and, importantly, being asymptomatic. The idea that one is healthy and fit without any symptoms and thus does not require any form of health check significantly hinders progress and presents a challenge not only for colorectal cancer but for many other medical issues as well.
While there have been improvements in disseminating information through mass media, social media, community talks, educational health fairs, and testimonials from past patients to raise awareness, more efforts are needed to educate the public on the importance of early screening in preventing the progression of polyps into cancers. A future with fewer advanced cancers would lead to reduced healthcare costs and improved overall health outcomes.
KEYWORDS:colorectal cancer, colorectal polyps, colorectal cancer screening, stool occult blood test, bowel preparation, colonoscopy, endoscopy, colonic polypectomy, endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD)
REFERENCES
https://www.thestar.com.my/news/nation/2024/07/08/88-of-msians-not-screened-for-colon-cancer
https://www.thestar.com.my/news/nation/2024/07/08/health-checks-can-save-you
Schedule a consultation with our Gastroenterologist & Physician, Dr. Chiam Keng Hoong today! Click here for appointment