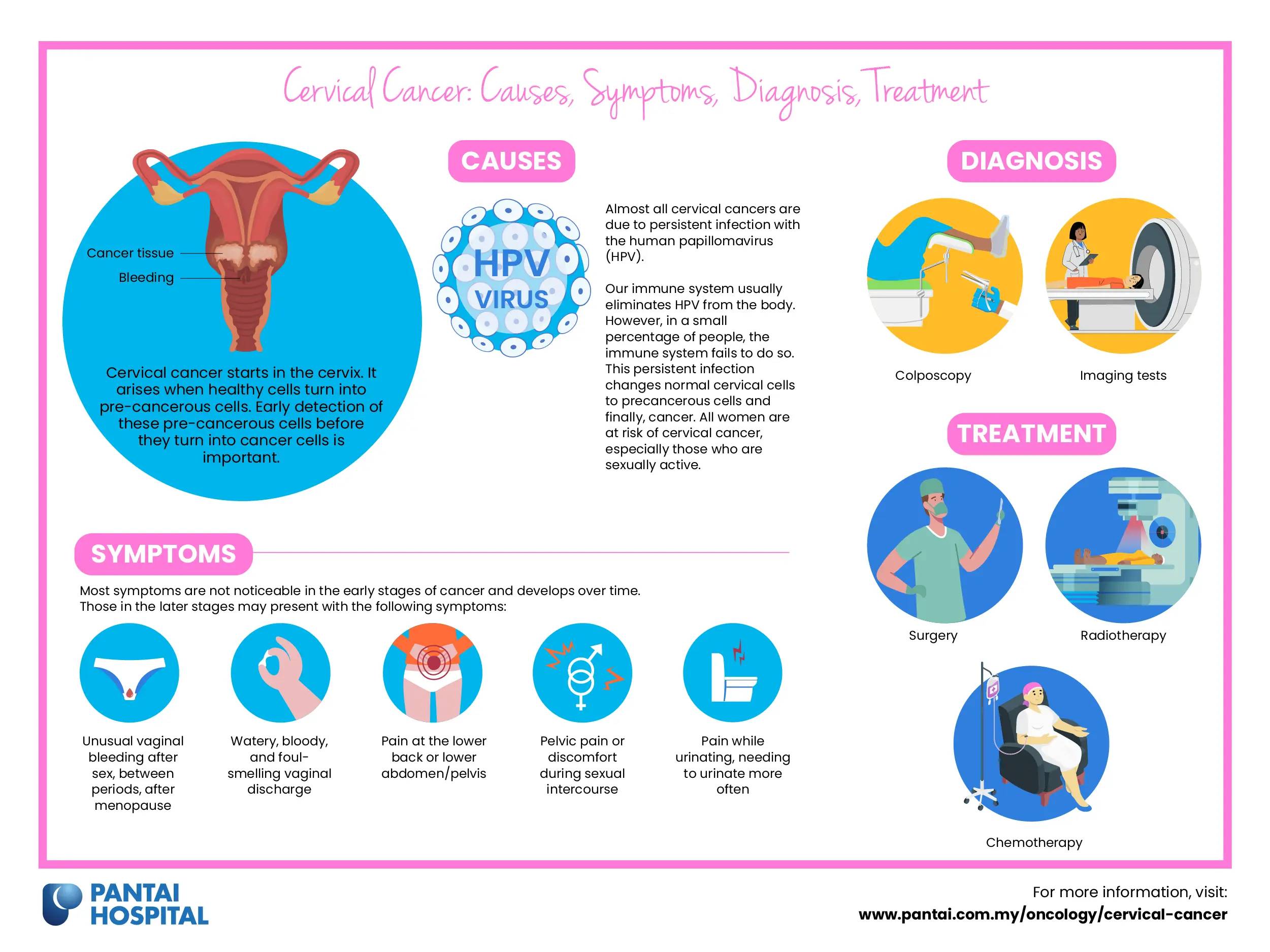
Cervical cancer starts in the cervix (the opening between the uterus and the vagina). It arises when healthy cells turn into pre-cancerous cells. Therefore, the early detection of these pre-cancerous cells before they turn into cancer cells is important.
Cervical cancer is one of the most prevalent cancers among Malaysian women and it typically affects women between the ages of 14 to 44 years.
What are the types of cervical cancer?
Cervical cancer occurs in the cervix or birth canal cells, which connect the uterus and the vagina. There are two types of cervical cancers, squamous cell carcinoma and adenocarcinoma. These are determined by the appearance of cells under a microscope.
- Squamous cell carcinoma originates in thin, flat cells lining the bottom of the cervix and accounts for 90% of cervical cancers.
- Adenocarcinoma originates in glandular cells lining the upper portion of the cervix and accounts for the remaining portion (10%) of cervical cancers.
What are the causes of cervical cancer?
Almost all cervical cancers are due to persistent infection with the human papillomavirus (HPV).
Our immune system usually eliminates HPV from the body. However, in a small percentage of people, the immune system fails to do so. This persistent infection changes normal cervical cells to precancerous cells and finally, cancer. All women are at risk of cervical cancer, especially those who are sexually active.
There are 14 high-risk HPV subtypes which can lead to the predisposition of cervical cancer. Infection with HPV, especially with HPV types 16 and 18, increases the risk of cervical cancer. The majority of HPV infections result from both penetrative sexual intercourse and non-penetrative sexual activity.
HPV infections typically do not cause physical symptoms. However, in certain individuals, these infections may lead to pre-cancerous lesions that if left untreated, can develop into cancers of the anus, cervix, vulva, and vagina in women.
What are the risk factors for developing cervical cancer?
The following factors increase the risk of developing cervical cancer:
- Human Papillomavirus (HPV) infection
- Human immunodeficiency virus (HIV) infection
- Having sexually transmitted infections such as chlamydia (caused by Chlamydia trachomatis bacteria)
- Having multiple sexual partners
- Weakened immune system caused by pre-existing health condition
What are the signs and symptoms of cervical cancer?
Most symptoms are not noticeable in the early stages of cancer and develops over time.
Those in the later stages may present with the following symptoms:
- Unusual vaginal bleeding after sex, between periods, after menopause
- Watery, bloody, and foul-smelling vaginal discharge
- Pain at the lower back or lower abdomen/pelvis
- Pelvic pain or discomfort during sexual intercourse
- Pain while urinating, needing to urinate more often
These symptoms can be caused by numerous other conditions, which are more common than cervical cancer. Therefore, Therefore, it is highly recommended for all women to routinely go for their screening test and consult a gynaecologist if you notice one or more of these symptoms.
How do doctors diagnose cervical cancer?
Your doctor would initially inquire about your general health and symptoms before conducting thorough physical and gynaecological tests. You may also require blood and urine tests.
Other diagnostic tests may include:
- Colposcopy
- Colposcopy is the primary test used to thoroughly examine the cervix for cervical cancer.
- A colposcope is a special magnifying glass used to examine the cervix's skin-like covering. It allows for the detection of changes or abnormalities that are too small to be seen by the human eye.
- A biopsy may be performed if an abnormal area is detected during a colposcopy. This would require the collection of a small sample of tissue to be sent for examination in a laboratory.
- Imaging tests
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- X-ray
Learn more about the different types of screening and diagnostic procedures performed to diagnose cervical cancer.
How is cervical cancer treated?
The course of treatment for cervical cancer is determined by stage and type of cancer. Key treatments include surgery, chemotherapy and radiotherapy.
- Surgery
Surgery is typically the main treatment method used if the cancer is detected early. The surgeries used in the treatment of cervical cancer include:
- Cervical conisation: Excision of a cone-shaped tissue sample from the cervix. It may be used in the diagnosis or treatment of cervical cancer.
- Trachelectomy: Removal of the cervix with some surrounding tissues. The uterus would still be left in place, so pregnancy may still be possible.
- Hysterectomy: Removal of the uterus and cervix in its entirety. Pregnancy would not be possible following this procedure.
- Pelvic exenteration: Removal of the fallopian tubes, ovaries, uterus, vagina, bladder, rectum, and part of the colon. This procedure is performed if the cancer has spread and cannot be effectively treated through other methods.
- Radiotherapy
Radiotherapy employs high-energy radiation to reduce the size of tumours and kill cancer cells. This procedure is used to alleviate the symptoms of advanced cancer. Radiotherapy may be used as the main method of treatment if the tumour is large or has spread.
There are two types of radiotherapy:
- External beam radiation (EBRT): Externally directing a radiation beam to the affected area.
- Brachytherapy: Briefly placing a device containing radioactive material inside or close to the vagina for a few minutes.
- Chemotherapy
Chemotherapy is a cancer treatment that involves intravenous administration of cytotoxic drugs via blood vessels for systemic circulation.
Learn more about the different types of treatment technologies to treat cervical cancer.
What can I do to reduce the risk of developing cervical cancer?
Vaccination and regular screening tests are the best ways to prevent cervical cancer.
- HPV vaccination
- Some forms of HPV infections can be prevented by vaccines. Vaccines cannot be used to treat an already existing HPV infection.
- The vaccine should typically be administered before a person is sexually active. Learn more about HPV vaccination in Malaysia to protect yourself from cervical cancer.
- Screening test
- A Pap test involves the collection of a sample of cells from the cervix to be tested for the presence of cancer and pre-cancer. It is regarded as a primary cervical cancer screening technique.
- Regular HPV screenings via Pap tests can prevent cervical cancers. All women who are sexually active should undergo regular screening with the pap test and/or HPV DNA test.
- It is recommended that women above 21 years of age get a pap test done once every three years.
- Other preventive steps
- Limit the number of sexual partners
- Use condoms during sexual activities
- Avoid smoking
Do I need to get screened for cervical cancer?
Early detection of cervical cancer occurs in nearly half of the cases, making it highly treatable. Therefore, the majority of women should be routinely screened for cervical cancer via a HPV test, Pap test, or a combination of the two. Women should be routinely screened once every few years once they turn 21.
Consult your doctor to determine if you would benefit from a cervical cancer screening.
Make an appointment at Pantai Hospitals
Early detection of cervical cancer makes it easier to treat the disease with effective and appropriate treatment. A dedicated multidisciplinary team of specialists and oncologists at Pantai Hospitals is available for consultation to provide the best care and assistance to patients through screening, diagnosis, and treatment.
Get in touch with us to book an appointment today if you have any concerns or questions about cervical cancer treatment options.
Pantai Hospitals have been accredited by the Malaysian Society for Quality in Health (MSQH) for its commitment to patient safety and service quality.

 Request an Appointment
Request an Appointment.webp?sfvrsn=276ce14_1/vector-(3).webp) International Patient
International Patient
.webp)

 Find A Doctor
Find A Doctor



.webp?sfvrsn=20763f7d_21)
.webp?sfvrsn=f2a2c343_12)